NEJM: 基因演化,从癌前病变到黑色素瘤
2015-11-14 Medsci MedSci原创
黑色素瘤进展期间伴随着一系列基因改变。研究展示不同黑色素瘤亚型的明显有区别的演化轨迹,识别了黑色素肿瘤一个中间类型,特点是存在一个以上致病基因改变和独特的组织病理学特征。研究还揭示出在黑色素瘤发生和发展过程中紫外线辐射都是一个主要因素。

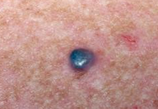
黑色素瘤(melanmoa)是一种极度恶性肿瘤,其特点是能产生黑色素,以30岁以上成年患者多见,常见发生部位是足底部以及外阴肛门部皮肤。黑色素瘤类型多变,可以原发即为恶性,也可以由癌前病变交界痣转化。近年来对于可以导致黑色素瘤的基因突变已有较深入研究,已知有多种致癌基因在黑色素瘤发生发展过程中起作用,然而科学家对这些基因在黑色素瘤中的演化顺序,何时起作用仍不清楚。
研究人员已经在很大程度上完成了黑色素瘤致病突变分类,然而这些突变发生的顺序不是很清楚。New Engl J Med 11月12日发布文章,重点研究致癌基因在黑色素瘤发生发展过程中的演化。
研究人员对37例原发黑色素瘤和转移瘤的150个病灶进行采样,对293个肿瘤相关基因进行测序。这些病灶的组织病理学结构性改变包括可以确定的良性病变,中间病变和表皮内或侵袭性黑色素瘤。
研究结果显示,癌前病变由突变基因激活,已知这些突变基因激活有丝分裂蛋白激酶途径。可以明确的良性病变组织存在独特BRAF V600E突变。而归类为中间类型的病变组织内含有丰富的NRAS突变和额外的随机突变。总共77%的中间类型病灶和原位黑色素瘤存在TERT启动子突变。发现TERT启动子突变表明。这些突变选择出现在意外的肿瘤进展早期阶段。CDKN2A等位基因失活只出现在侵袭性黑色素瘤。PTEN和TP53突变只在进展性原发性黑色素瘤发现。点突变促使病变逐渐演化,从良性到中间类型直到黑色素瘤。全部演化阶段都与可探测的紫外线辐射效应有很强的特征性标记。只在侵袭性黑色素瘤中发现基因组的普遍改变。随着黑色素瘤进展,肿瘤异质性得以显现,各个肿瘤亚群的基因构成明显不同。
这项研究定义了黑色素瘤进展期间伴随着一系列基因改变。展示不同黑色素瘤亚型的明显有区别的演化轨迹。研究识别了黑色素肿瘤一个中间类型,特点是存在一个以上致病基因改变和独特的组织病理学特征。研究还揭示出在黑色素瘤发生和发展过程中紫外线辐射都是一个主要因素。
原始出处
1. Hunter Shain, Iwei Yeh, Ivanka Kovalyshyn, et all. The Genetic Evolution of Melanoma from Precursor Lesions. N Engl J Med 2015;373:1926-1936.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
70
#色素#
26
很,很值得好学习
119
#黑色素#
29
#黑色素#
20