J Thorac Oncol: 探索肺癌生存率性别差异的预后因素
2022-02-05 yd2015 MedSci原创
研究表明,性别相关的肺癌生存差异很大程度上是由已知的预后因素所决定的,这表明有机会探索治疗偏好、选择和可及性方面的性别差异。
有研究表明,女性患肺癌后的存活时间往往比男性长;然而,这种性别差异的潜在驱动因素在很大程度上仍然难以捉摸。因此,有来自澳大利亚的团队开展了相关研究,评估与肺癌生存率的性别差异相关的因素。成果发表在Journal of Thoracic Oncology杂志上。
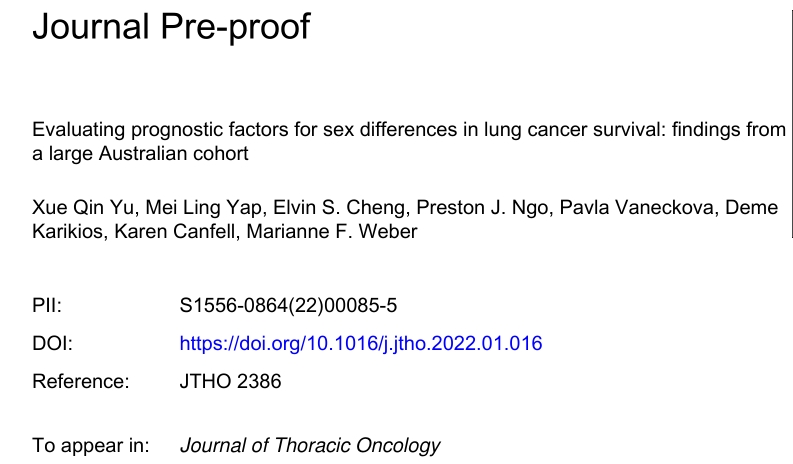
1130例患者纳入本研究分析,包括488名女性和642名男性。与男性患者相比,女性肺癌生存期更长(中位OS:1.28 vs 0.77年,p<0.0001)。
亚组分析显示,在组织学不同亚型分析,比如腺癌、小细胞肺癌(SCLC)和其他亚型中,女性肺癌生存期较男性的更长(p<0.0001);

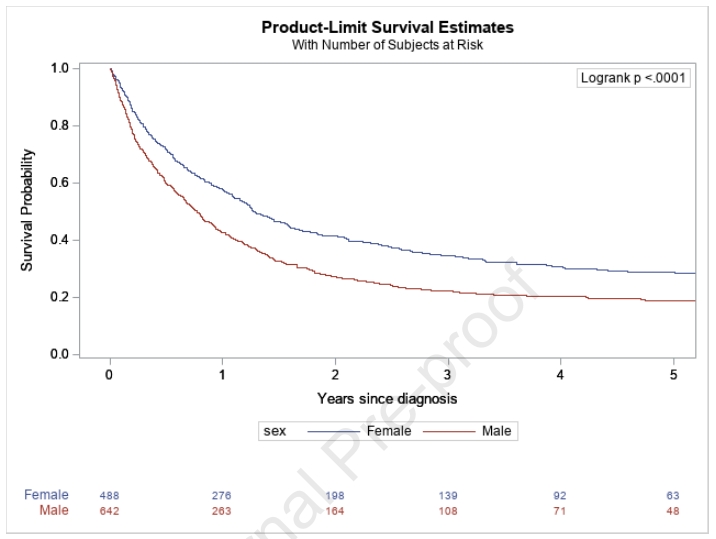
肿瘤分期,比如局部分期,非局部分期和未名分期等方面,女性肺癌生存期较男性的更长(p<0.0001);
肿瘤的治疗与否中,也观察到女性肺癌生存期较男性的更长(p<0.0001);

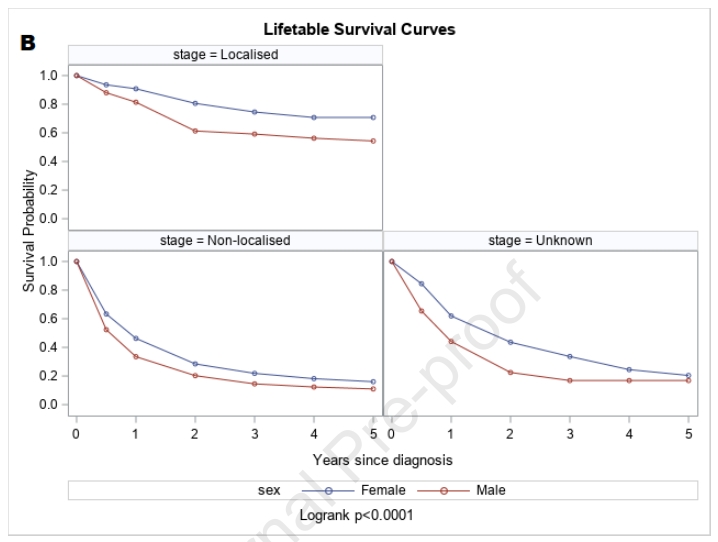
吸烟和未吸烟患者中,也观察到女性肺癌生存期较男性的更长(p<0.0001)。
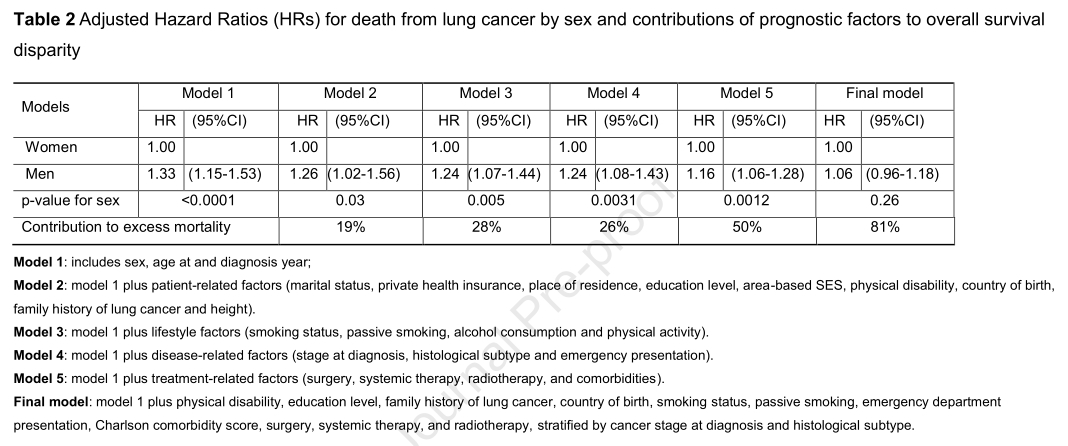
在单变量回归分析中,男性肺癌死亡风险显著高于女性(HR 1.43, 95% CI 1.25-1.64;术中,0.0001)。经过最小的调整(年龄和诊断年份),死亡的额外风险降低到33% (HR 1.33, 95% CI 1.15- 1.53)。同时经过其他因素调整后,男性患者的死亡风险有所下降,但是仍高于女性患者。
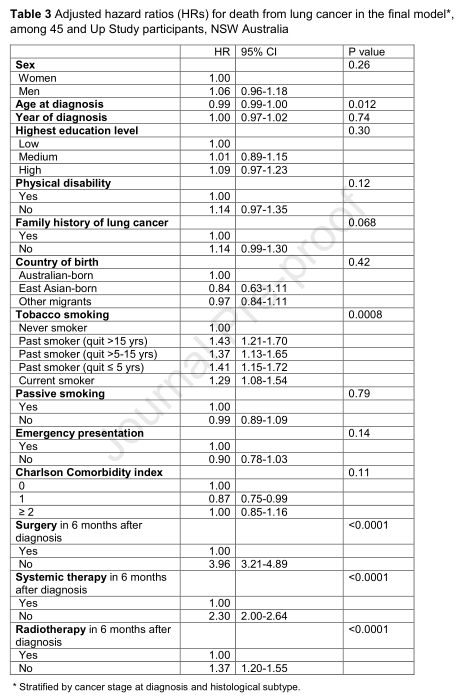
综上,研究表明,性别相关的肺癌生存差异很大程度上是由已知的预后因素所决定的,这表明有机会探索治疗偏好、选择和可及性方面的性别差异。
原始出处:
Xue Qin Yu, Mei Ling Yap, Elvin S Cheng, et al. Evaluating prognostic factors for sex differences in lung cancer survival: findings from a large Australian cohort. Journal of Thoracic Oncology. DOI: https://doi.org/10.1016/j.jtho.2022.01.016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#THORAC#
48
#Oncol#
40
#生存率#
41
#预后因素#
47
学习了
55
非常实用
49