盘点:房颤研究汇总
2016-10-06 MedSci MedSci原创
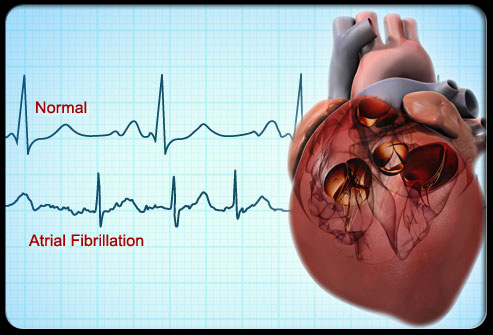
心房颤动(简称房颤)是最常见的持续性心律失常。随着年龄增长房颤的发生率不断增加,75岁以上人群可达10%。房颤时心房激动的频率达300~600次/分,心跳频率往往快而且不规则,有时候可达100~160次/分,不仅比正常人心跳快得多,而且绝对不整齐,心房失去有效的收缩功能。房颤患病率还与冠心病、高血压病和心力衰竭等疾病有密切关系。这里小M整理了2016年以来关于房颤的最新研究汇总,与大家分享。【
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











值得学习。
45
值得学习。
48
继续关注!
61
谢谢分享!
55
好文章,受益
70
总结的很好!
37
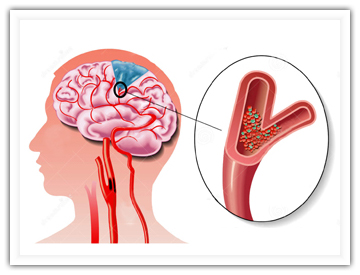
房颤并发脑梗塞!
26
心房颤动(简称房颤)是最常见的持续性心律失常!!
29
谢谢,学习知识
26
学习了谢谢。
32