Eur J Endocrinol:石蜡标本转录组分析在肾上腺皮质癌诊断和预后中的价值
2022-03-19 从医路漫漫 MedSci原创
肾上腺皮质癌(ACC)是一种罕见的内分泌癌(每年每百万人中有1-2例),总体预后较差。诊断对患者管理至关重要,但由于这种疾病的罕见,诊断很困难。
背景:肾上腺皮质癌(ACC)是一种罕见的内分泌癌(每年每百万人中有1-2例),总体预后较差。诊断对患者管理至关重要,但由于这种疾病的罕见,诊断很困难。事实上,在肾上腺皮质肿瘤(ACT)中,ACC是罕见的,大多数是肾上腺皮质腺瘤(ACA)。病理恶性肿瘤评分称为Weiss评分,最常用于诊断。然而,具有中等评分和罕见组织学变异的肿瘤不容易被分类。特别是,确定由大细胞和嗜酸性颗粒组成的嗜酸性变异体的恶性是具有挑战性的。
ACC的5年总体生存率一般低于40%,但异质性。预后分层对指导治疗决策很重要,特别是在辅助治疗。临床上使用的主要预后因素是肿瘤分期Ki-67增殖指数。其他预后因素通常包括皮质醇分泌和年龄。
以前的基因组研究表明,基因组变化集中在不同的分子亚型。转录组图谱是分子分类的基石。转录组图谱将肾上腺皮质腺瘤与癌区分开来,并鉴定出两组与预后密切相关的ACC:“C1a”亚组,其增殖基因过度表达,预后不良;“C1B”亚组,具有免疫特征,预后较好。从转录组特征,已推断出特定的mRNA标记,如BUB1BPINK1的差异基因表达。这些靶向标记物改善了ACC的诊断和预后评估。然而,到目前为止,转录组图谱及其靶向替代标记物仅限于高质量的肿瘤RNA,需要高质量的冰冻组织样本。在常规实践中,获取这种类型的材料要求很高,而对于ACC患者来说,往往无法实现。
最近的3’RNA测序技术捕获并测序了多腺苷化RNA 3’端的短片段,这些片段不太容易被RNA降解。与基因表达微阵列或标准的全长RNA测序不同,这种技术只需要少量和低质量的RNA,与福尔马林固定石蜡包埋(FFPE)样本兼容。
目的:主要目的是利用新的3’端RNA测序技术,确定福尔马林固定石蜡包埋(FFPE)样本的转录组图谱。第二个目的是通过重点研究罕见的嗜酸细胞ACT变体,展示这种技术探索大型FFPE档案的能力。
方法:我们纳入131例ACT:来自科钦医院的训练队列和来自维尔茨堡医院的独立验证队列。用QuantSeq(Lexogen)和NextSeq500(Illumina)从FFPE样本中产生3’转录组。
结果:在训练队列中,无监督聚类识别出3组:“C1A”型侵袭性癌(N=28,29%)、“C1B”型癌(N=28,29%)和“C2”型腺瘤(N=39,41%)。FFPE转录组的预后价值在验证队列中得到证实(5年OS:C1a组为26%(N=26),C1B组为100%(N=10),p=0.003)。在包括肿瘤分期和Ki-67的多变量模型中,FFPE转录组是一个独立的预后因素(OS-HR 7.5,p=0.01)。嗜酸性粒细胞ACT(N=19)未形成任何特异簇。嗜酸细胞癌(N=6)和恶性潜能未明的嗜酸性细胞癌(N=4)均为“C1B”。
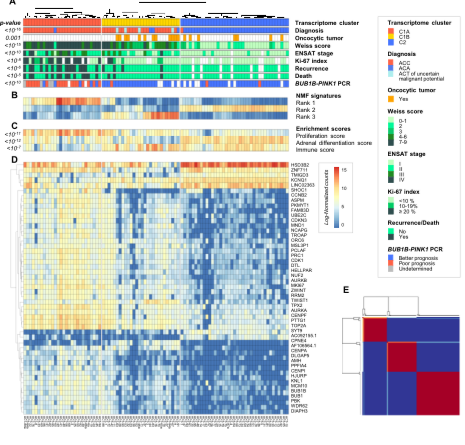
图1.训练队列中ACT的FFPE转录组分类A.基于2000个最易变的基因对ACT的非监督分类确定了三个主要组,对应于“C1A”侵袭性癌、“C1B”惰性癌和“C2”腺瘤。B.用于生成非监督分类的3个非负矩阵分解(NMF)等级的热图。激素(肾上腺分化)、增殖和免疫征象在每种ACT中的表达。D.三组转录组中差异最显著的前50个基因的表达谱。即通过迭代聚类算法表示样本之间的相似度的一致性矩阵。行和列是患者样本。共识矩阵值的范围从0(从不聚在一起)到1(始终聚在一起)。

图2.不同肿瘤区域的FFPE转录组分类。对训练队列中5名患者的两个不同肿瘤区域进行苏木精/伊红/赛弗兰染色(放大40倍),其中一个为侵袭性(-a)区,一个为非侵袭性(-b)区。黑条代表50微米。黑色箭头表示有丝分裂。白色箭头表示不典型的有丝分裂。B.描述为5名患者采样的两个不同的肿瘤区域,其中一个是侵袭性(-a),另一个是侵袭性(-b)。不适用:Fuhrman核级不适用于嗜酸性细胞。C.基于PCA的两个主成分(Dim1、Dim2)的样本投影基于训练队列的95个独特患者中的2000个最可变基因。来自训练队列的样本显示为转录组班级着色的模糊圆圈。来自两个不同肿瘤区域的8名患者的样本按患者的颜色显示为全三角形。
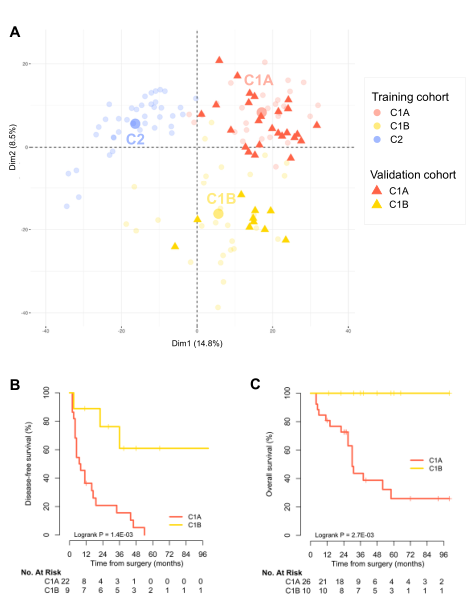
图3.ACC验证队列中的FFPE转录组分类和预后A.样本投影基于PCA的两个主成分(Dim1,Dim2),基于训练队列中95个独特患者中最可变的2000个基因。来自训练队列的样本显示为转录组班级着色的模糊圆圈。来自验证队列的样本以转录组类别着色的完整三角形表示。B.根据验证队列中I-III期ACC患者的预测转录组类型进行无病生存。根据验证队列的I-IV期ACC患者的预测转录组分类,总的存活率。
结论:3’RNA测序法是从FFPE样本中确定ACT分子类型的一种简便方法。这项技术应该有助于常规使用和大型回顾研究。
原文出处:Jouinot A, Lippert J, Sibony M,et al.Transcriptome in paraffin samples for the diagnosis and prognosis of adrenocortical carcinoma.Eur J Endocrinol 2022 Mar 01
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肾上腺皮质癌#
48
#肾上腺#
54
#标本#
30
#转录组分析#
38
#转录#
45
#转录组#
35