CBCT辅助诊断上颌**磨牙罕见双腭根1例
2020-06-16 关晶 谷建琦 张栋 现代口腔医学杂志
根管治疗是目前对牙髓炎、根尖周炎最理想的治疗方法。根管治疗中,额外牙根或根管的遗漏是导致治疗失败的重要原因。所以,对根管系统的准确判断和必要的辅助检查是根管治疗成功的关键。上颌第一恒磨牙多为独立的三个
根管治疗是目前对牙髓炎、根尖周炎最理想的治疗方法。根管治疗中,额外牙根或根管的遗漏是导致治疗失败的重要原因。所以,对根管系统的准确判断和必要的辅助检查是根管治疗成功的关键。上颌第一恒磨牙多为独立的三个牙根,分别是近颊根、远颊根、腭根,常见3~4个根管,其中近中颊根较易出现双根管且研究报道较多。对于腭侧牙根变异的相关报道较少。本文报告上颌第一磨牙双腭根1例,为上颌第一磨牙解剖变异的诊断及治疗提供参考经验。
1.病例资料
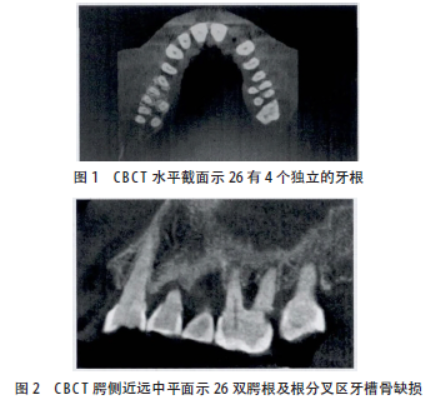
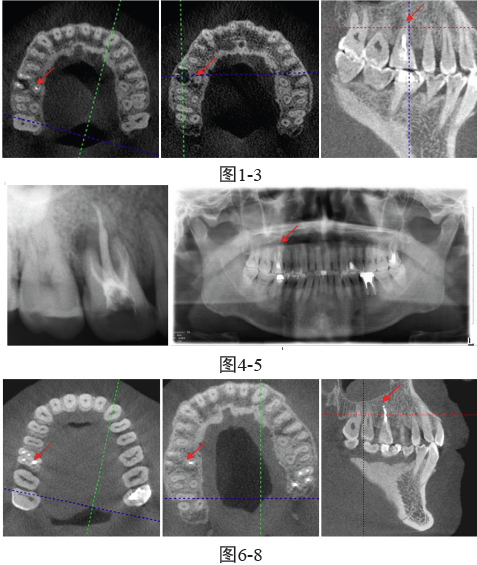
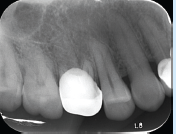
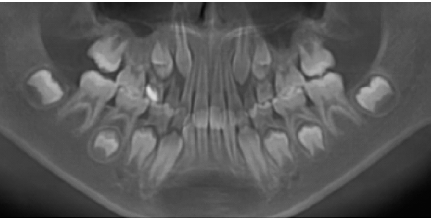
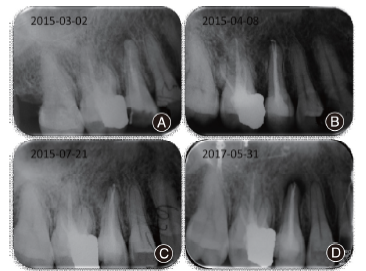
患者,女,69岁,因要求种植修复左下后牙来我院就诊。对患者进行口腔全面检查时发现患者26腭侧牙颈部龋坏,腭侧近龈缘处牙龈溢脓。探诊可探及腭侧正中根分叉及深的牙周袋。无松动、无扣痛及冷热痛。牙髓活力测定仪显示牙髓有活力。口腔锥体束CT(cone beam computed tomography,CBCT)显示26具有罕见的四个完全分开的牙根,其中两个颊根,两个腭根。根分叉下方可见骨质破坏。而对侧的16为常见的三根牙。诊断为26牙颈部中龋,牙周炎。治疗:去腐、备洞、树脂充填。牙周龈上洁治、龈下刮治,派丽奥牙周上药。经数次的牙周治疗,牙周状况明显好转。
2.讨论
上颌第一磨牙的双腭根发生率极低。1991年,Christie等在国际上第一次报道了上颌第一磨牙双腭根。近年来,国内学者开始通过CBCT在中国患者中发现上颌第一磨牙的双腭根。景亚楠等对630颗上颌第一磨牙进行CBCT图像分析发现4根发生率为0.48%。杨博等对1957颗上颌磨牙CBCT图像分析发现上颌第一磨牙双腭根的发生率为0.31%。多为双侧对称。而本病例为单侧变异,更为罕见。目前临床使用的锥形束CT(cone-beam computed tomography,CBCT)图像分辨率高,可提供三维影像,能观察到传统X线片难以辨别的结构。
近年来,CBCT在临床上逐渐得到广泛运用,可从矢状面、冠状面以及横断面对根管进行精确的形态学分析。这为变异牙根的发现及疑难根管的治疗提供了直观而准确的信息。提高了根管治疗的成功率。通过查找文献,笔者发现上颌磨牙双腭根多分叉较大,根柱较短。极易出现牙周病和根分叉龋坏,增加了治疗难度。
本病例也是这种情况,初诊时发现腭侧牙龈溢脓,腭侧牙颈部大量食物残渣,肿胀的牙龈和食物残渣覆盖了腭侧的龋坏和腭根分叉。随着充填和牙周数次治疗,牙周状况好转,腭侧根分叉暴露,以利于患者的牙周维护。临床医师在诊疗过程中要对解剖变异的牙齿有所警惕,本病例也提示我们定期进行口腔检查更能有效预防由于牙齿解剖变异造成的牙体牙周疾病。合理利用CBCT等影像手段,明确诊断、提高临床治疗的成功率。
原始出处:
关晶,谷建琦,张栋.CBCT辅助诊断上颌第一磨牙罕见双腭根1例[J].现代口腔医学杂志,2019,33(03):187+189.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#双腭根#
39
#CBCT#
43
#罕见#
29
#磨牙#
42
#上颌#
51