Nano Today:浙大二院发文提出脑胶质母细胞瘤的新疗法——化学动力学治疗!
2022-03-07 浙江大学医学院 网络
脑胶质母细胞瘤(GBM)是神经外科领域治疗难度最高的中枢神经系统恶性肿瘤,每十万人中约有3-5人发病。
近日,浙江大学医学院附属第二医院神经外科张建民团队在国际知名期刊《Nano Today》上发表题为"Localized NIR-II laser mediated chemodynamic therapy of glioblastoma"的研究文章,提出了一种近红外二区激光介导的化学动力学治疗脑胶质母细胞瘤的一种新方法。
脑胶质母细胞瘤(GBM)是神经外科领域治疗难度最高的中枢神经系统恶性肿瘤,每十万人中约有3-5人发病。具有难治疗、易复发、致死率高等特点,即使手术加上术后放化疗,其GBM患者的中位生存期也只有约16个月,给患者及其家庭带来了沉重的负担和灾难,也对人类健康带来严重影响。因此,探索如何改善GBM诊疗现状的新方法,提高GBM的治疗效果一直是当今医疗领域的重大挑战和研究课题。
活性氧(ROS),包含羟基自由基(·OH)、过氧化氢(H2O2)、单线态氧和超氧阴离子等,可以损毁胞内DNA、蛋白和脂质等生物分子进而有效地杀死肿瘤细胞。近年来,研究者们基于ROS发展了不同的肿瘤治疗策略,其中比较典型的就是化学动力学治疗(CDT),后者可以利用基于金属离子的芬顿或类芬顿反应将活性较低的H2O2转换为毒性更强的·OH,诱导产生氧化应激进而杀伤肿瘤细胞。
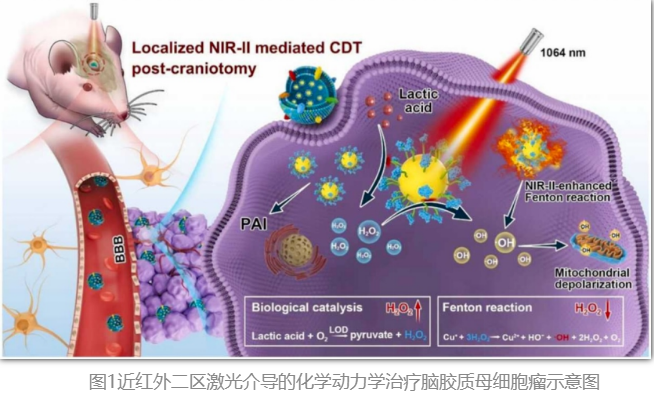
本研究首先制备一种超小的硒化铁亚铜纳米晶体(CuFeSe2 NCs),进而偶联乳酸氧化酶(LOD),再利用修饰GBM细胞膜蛋白的仿生脂质体膜对纳米晶体进行包覆,获得了一种仿生纳米催化反应器(CLLC)。CLLC通过尾静脉注射后,可以跨越血脑屏障并精准靶向原位GBM。CLLC进入GBM细胞后可以发生基于亚铜离子的类芬顿反应,催化过氧化氢(H2O2)产生毒性更强的羟基自由基(·OH)对GBM进行化学动力学治疗(CDT),LOD可以催化细胞内过量的乳酸产生H2O2为CDT提供原料。此外,开放小鼠颅骨骨窗以提高近红外二区激光(NIR-II laser)照射效率,由于具有高光热转换效率,CLLC可以在NIR-II laser照射下产生良好的光热升温效应,温和的升温效应可以进一步增强CDT效率。
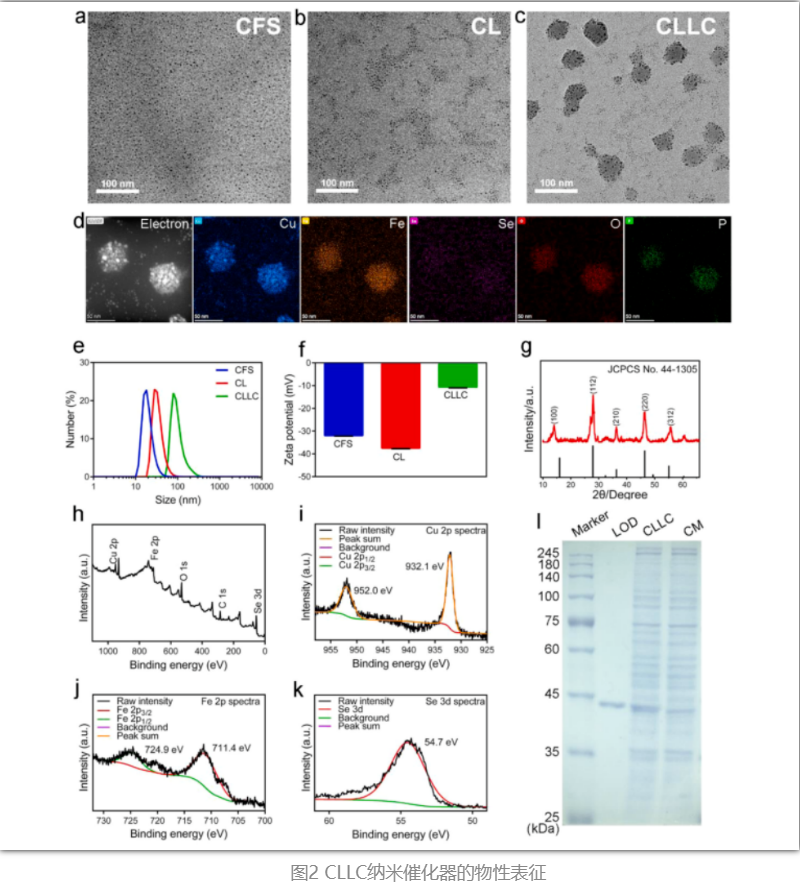
通过TEM、DLS、XPS、XRD、SDS-PAGE等实验证明CLLC的成功制备。此外,LOD的偶联以及仿生脂质体膜的包覆不影响CuFeSe2 NCs的晶型与元素价态。
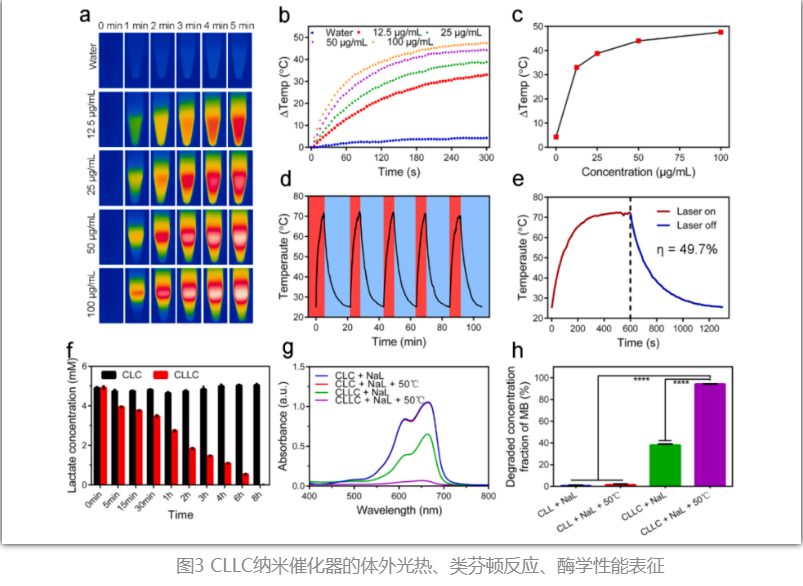
CLLC具有良好的光热转换效率,在NIR-II laser照射下可以使溶液快速升温;CLLC中的LOD可以发挥酶学作用,在体外可以催化乳酸钠产生H2O2;CLLC中的亚铜离子可以发挥类芬顿反应,催化H2O2产生·OH,反应溶液温度升高和LOD催化产生的H2O2可以增强该类芬顿反应。
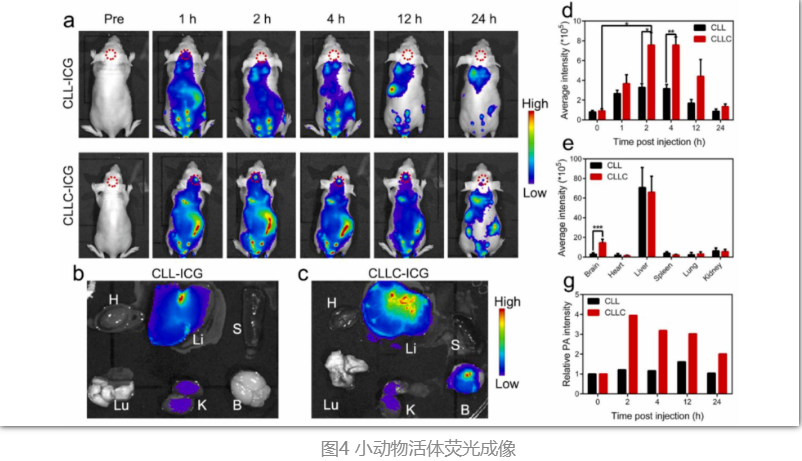
通过吲哚菁绿(ICG)标记后,进行小动物活体荧光成像来评估CLLC的体内靶向效果,发现小鼠脑内GBM的荧光信号在尾静脉注射CLLC-ICG 2小时后达到峰值,并维持高信号至12小时,表明发现CLLC可以高效地跨越血脑屏障并主动靶向原位GBM。
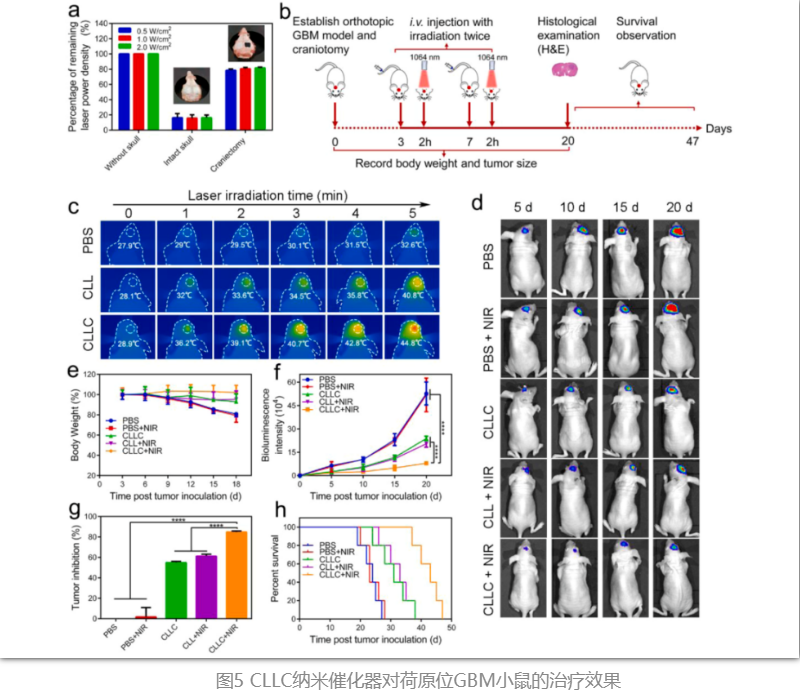
同时,为提高NIR-II laser照射至脑内GBM的效率,开放小鼠的颅骨骨窗;在NIR-II laser照射下,CLLC介导的CDT对GBM显示出良好的治疗效果,在治疗20天后,肿瘤抑制率达到了84.9%,中位生存时间也明显增加(43天)。
综上,这种基于仿生纳米催化反应器实现原位NIR-II laser介导的增强CDT策略,为GBM的治疗提供了新的思路。
本研究创新点显示:
1. 原位NIR-II laser介导的增强CDT与温和光热作用用于GBM治疗;
2. CLLC纳米催化器可以跨越血脑屏障并主动靶向GBM,且具有非常低的脑毒性;
3. LOD可以催化肿瘤微环境中高表达的乳酸产生产生H2O2,为CLLC的类芬顿反应提供原料。
浙大二院神经外科为该论文的第一通讯单位,浙大二院神经外科博士生潘渊博为该论文的第一作者,浙大二院神经外科张建民主任、中科院宁波材料所慈溪生物医学工程研究所吴爱国研究员、李娟研究员、以及新加坡国立大学陈小元教授为本文的共同通讯作者。上述研究工作得到了国家自然科学基金、浙江大学教育部脑与脑机融合前沿科学中心、中国科学院青年创新促进会、宁波市科技局以及NUS School of Medicine Nanomedicine Translational Research Programme的资助与支持。
原始出处:
Yuanbo Pan, Canxin Xu, Hongzhang Deng, Qing You, Chenyang Zhao, Yanying Li, Qianqian Gao, Ozioma Udochukwu Akakuru, Juan Li, Jianmin Zhang, Aiguo Wu, Xiaoyuan Chen,Localized NIR-II laser mediated chemodynamic therapy of glioblastoma,Nano Today,Volume 43,2022,https://doi.org/10.1016/j.nantod.2022.101435.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#胶质母细胞#
33
#母细胞瘤#
38
#细胞瘤#
36
#浙大#
52
#新疗法#
46