CIHFC 2016:黄峻:慢性心力衰竭的药物治疗新进展
2016-03-12 小M MedSci原创
在2016 中国国际心力衰竭大会暨中国医师协会心力衰竭专业委员会第一届学术年会上,本届大会的共同主席、南京医科大学第一临床医学院黄峻院长做了题为“慢性心力衰竭的药物治疗新进展”的精彩报告。下面是MedSci对其报告内容的整理: 上世纪50-60开始应用利尿剂和地高辛治疗心衰,心衰的症状得以有所改善,此后的半个世纪心衰的治疗经历了3次重大转变。 第一阶段:血液动力学阶段(上世纪70-
在2016 中国国际心力衰竭大会暨中国医师协会心力衰竭专业委员会第一届学术年会上,本届大会的共同主席、南京医科大学第一临床医学院黄峻院长做了题为“慢性心力衰竭的药物治疗新进展”的精彩报告。下面是MedSci对其报告内容的整理:
上世纪50-60年代开始应用利尿剂和地高辛治疗心衰,心衰的症状得以有所改善,此后的半个世纪心衰的治疗经历了3次重大转变。
第一阶段:血液动力学阶段(上世纪70-90年代)
认识:认为心衰是心肌收缩力减弱,心脏前后负荷压力、容量及阻力增加的结果;
治疗:改善血液动力学
药物:正性肌力药物、血管扩张剂、利尿剂
1、正性肌力药物:多增加心衰患者死亡率
1991年发表在NEJM上的PROSIME研究1088例NYHA心功能Ⅲ-Ⅳ级慢性心衰患者随机接受米力农或安慰剂治疗,随访6个月,结果发现米力农组患者血流动力学参数得到了改善,但是死亡率确较安慰剂组增高了28%。正性肌力药物中只有地高辛不增加心衰患者的死亡率(参考DIG试验)。
2、血管扩张剂:不能使心衰患者获益
非二氢吡啶类长效钙拮抗剂氨氯地平的PRAISE1、2试验表明,其不仅不能改善心衰患者预后,还可激活RAAS和交感神经系统,有可能促进心肌重构和心衰发展。长期使用会增加患者病死率,因此不适宜长期用药。
3、利尿剂:可改善心衰症状,无改善预后的证据
急性失代偿中不可或缺
中度和重度心衰的长期治疗中不可或缺
对症疗法
无已证实的预后获益证据
使用可以的最低剂量来维持稳定性患者的正常血容量(干重)
小结:
血液动力学阶段——症状改善,死亡率未减少
第二阶段:神经体液阶段(20世纪90年代至2010年)
认识:认为RAAS和交感神经系统的过度激活导致心肌重构,是心衰发生和发展的主因
治疗:目的抑制过度激活的神经内分泌系统
药物:阻断RAAS的ACEI、ARB和醛固酮拮抗剂和阻断交感神经的β受体阻滞剂
既往的基础研究已经证实,RAAS和交感激活在心衰发展中起重要作用:高血压等危险因素造成初始的心肌损伤;RAS和交感神经系统过度兴奋,导致神经内分泌和细胞因子激活,进而促进重构,加重心肌损伤和心功能恶化,二者间的恶性循环,长期影响心肌功能,时心功能失代偿,导致心衰的产生。因此,阻断神经内分泌(主要为RAAS和交感)过度激活是防治心衰的关键。
1、ACEI:临床研究一致证实ACEI可降低心衰死亡和住院风险
CONSENSUS研究、SOLVD治疗研究、SOLVD预防研究、Overview研究、ATLAS研究等均证实ACEI可降低心衰死亡和住院风险。另外,一项纳入了32项随机、安慰剂对照、研究周期至少8周的ACEI临床研究的荟萃分析,采用意向处理评估总死亡率,和因心衰住院或死亡的情况。发现:CEI组,总死亡率降低了23%,因心衰住院或死亡降低了35%。
2、β受体阻滞剂:众多研究一致证实可降低心衰死亡和住院风险
临床研究荟萃分析证实治疗心衰非常有效:22个随机对照试验的荟萃分析,共包括10135例患者,结果发现β受体阻滞剂组的全因死亡率下降了35%,心血管死亡率下降了40%,心脏性猝死率下降了45%。
但是,β受体阻滞剂的适应症包括:
所有慢性收缩性心衰,病情相对稳定,LVEF小于或等于40%者,均必须终身使用,除非有禁忌症或不能耐受(1类,A级)
NHYA 1-3,需终身使用,除非有禁忌症或不能耐受
NHYAIVa,病情稳定后使用
阶段B、C、D,常规应用
阶段A,酌情应用
3、醛固酮拮抗剂:螺内酯降低心衰患者的全因死亡率30%(重要)
一项纳入了1663例患者、15个国家,195个中心的研究,随机双盲分组,发现小剂量螺内酯降低心衰全因死亡率30%(P<0.001),螺内酯组减少因心衰住院患者人数30%(P<0.001),因心死亡和住院的复合终点减少32%(P<0.001)。另外,EMPHASIS-HF研究也表明:醛固酮拮抗剂使NYHA Ⅱ级且LVEF小于等于35%的心衰患者显著获益。
心肌重构很重要的一个过程是心肌纤维化,而醛固酮在心肌纤维化过程中起着很重要的作用,而其他的治疗药物,即使是应用RAAS阻滞剂+β受体阻滞剂治疗后,醛固酮依然会产生。
小结:
神经体液阶段:预后改善,病死率仍较高
心衰治疗情况仍不乐观:
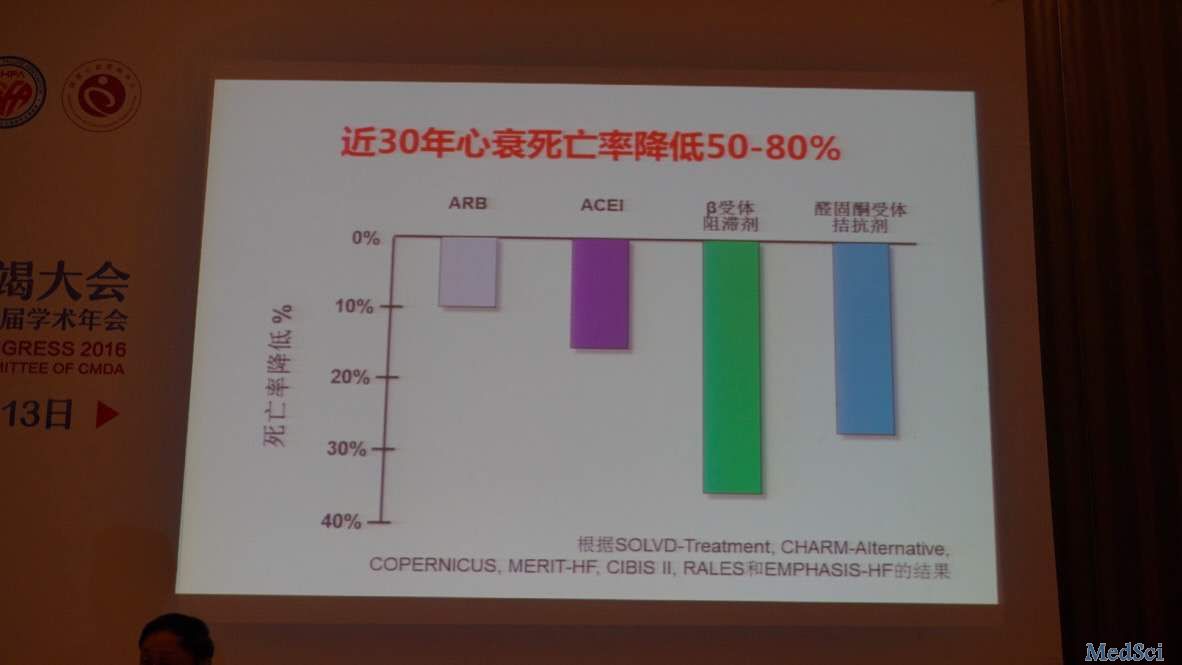
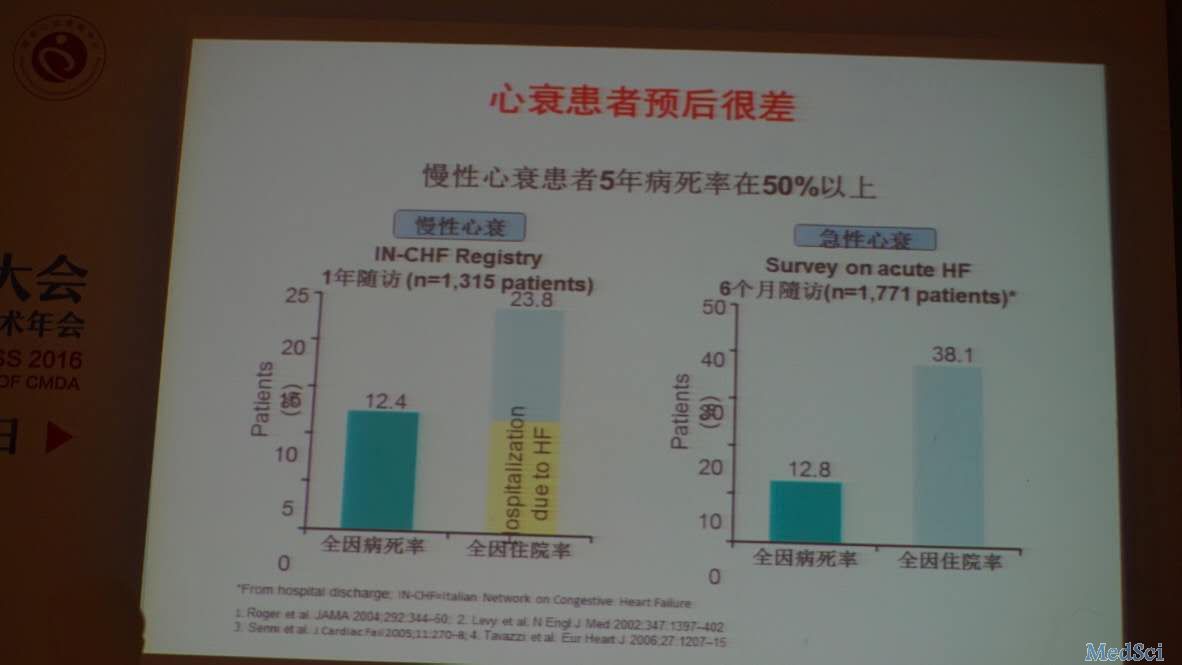
虽然近三十年心衰死亡率降低了50-80%(图1反映了各种神经体液阶段药降低的死亡率百分比),但是,根据2011英国国家心血管预后研究所(NICOR)心衰审计报告的结果,我们发现,心衰患者出院后1年全因死亡率高达33%,即使应用RAAS阻滞剂+β受体阻滞剂治疗后,1年全因死亡率仍超过20%。而慢性心衰患者5年病死率在50%左右。
上图是慢性心衰患者和急性心衰患者,治疗后病死率的研究结果
因此,心衰的治疗依然需要更多的研究,需要寻求其他的治疗药物。
第三阶段:整体调节和多靶点作用阶段(目前)
认识:认识到单纯应用神经内分泌阻滞剂存在局限性
治疗:神经内分泌和多靶点整体调节
药物:降低心率(依伐布雷定)、神经内分泌调节剂(LCZ696)、多靶点药物(如中药芪苈强心胶囊)
1、依伐布雷定(SHIF研究):单纯降低窦性心律
自从2010年的SHIF研究证实其有效(降低主要复合终点18%),2012年即被欧洲指南推荐,2014年开始被国内指南推荐使用,依伐布雷定已于去年在中国和美国上市。
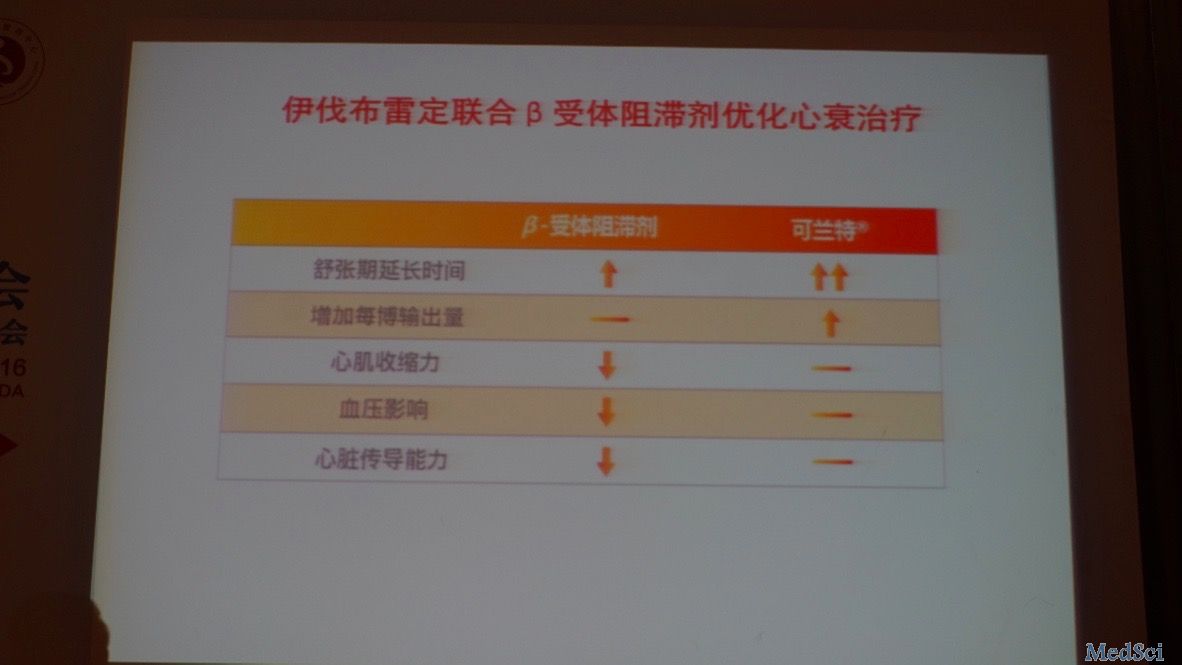
在这里要注意依伐布雷定与β阻滞剂的差异:依伐布雷定是特异性心脏起搏电流抑制剂,不影响房室传导;而且其只是单纯降低窦性心律,对血压无影响、不影响心肌收缩率。
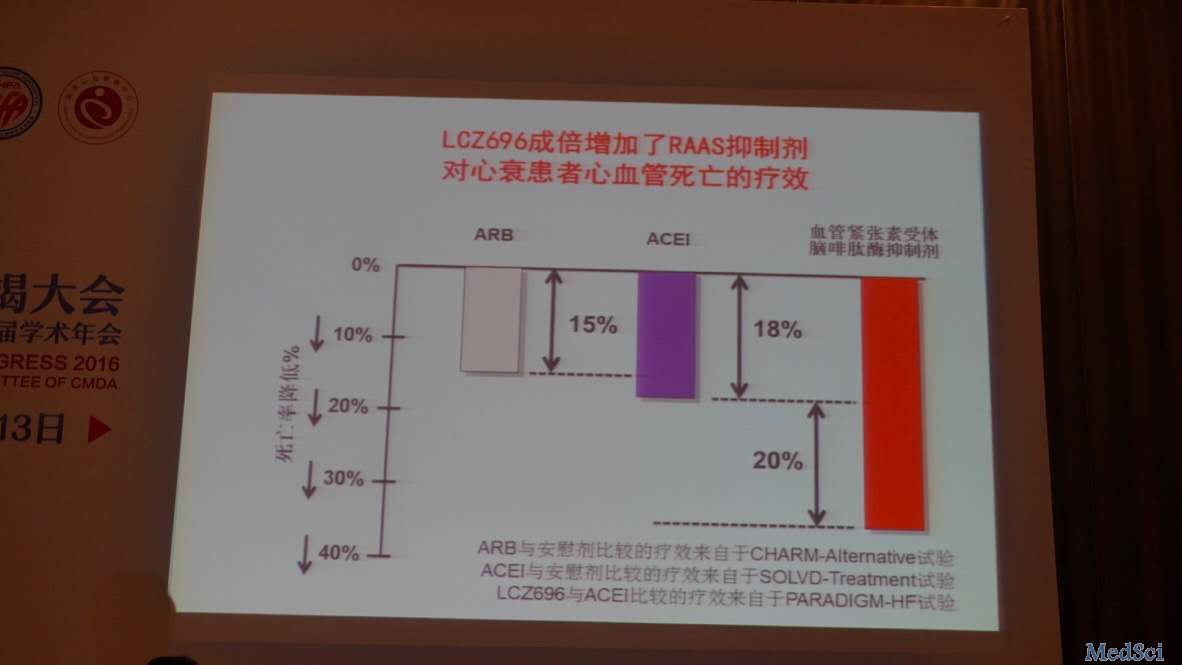
2、LCZ696:一个新型血管紧张素受体脑啡肽酶抑制剂
PARADIGM研究结果表明:LCZ696成倍增加了RAAS抑制剂对心衰患者心血管死亡的疗效,而且不良事件较少、较轻。
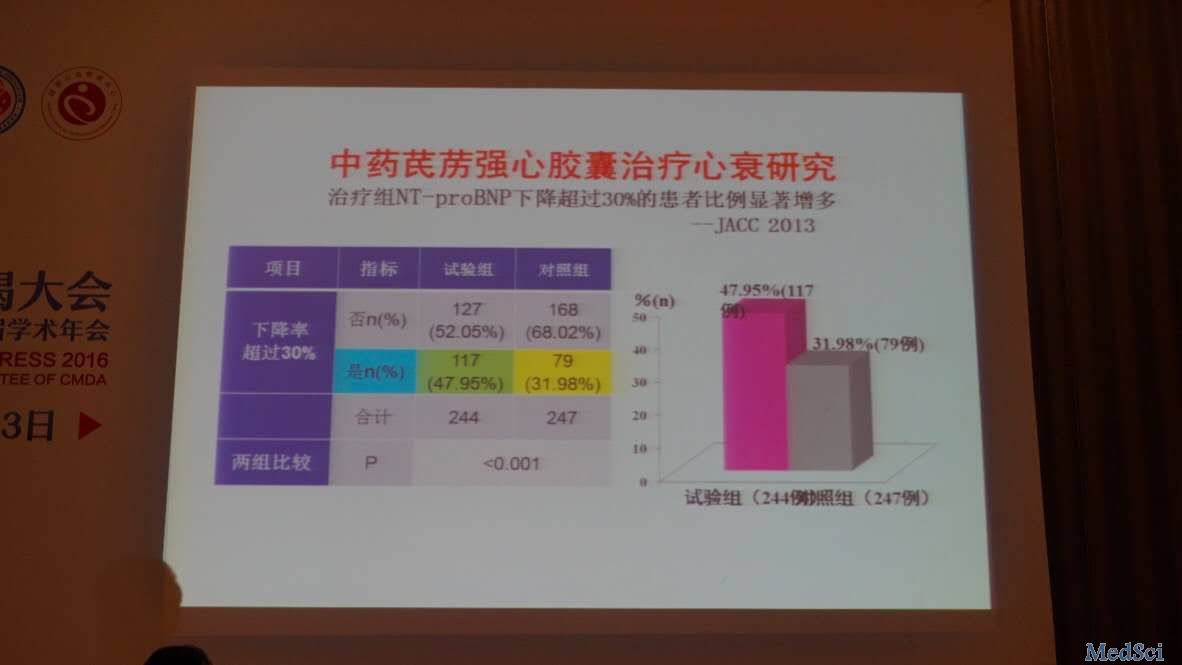
3、多靶点药物治疗:如中药芪苈强心胶囊
被评为JACC年度优秀论文的芪苈强心胶囊研究表明:试验组NT-proBNP下降超过30%的患者比例显著增加(将近一半)。
小结:
整体调节和多靶点作用阶段——治疗更优化,预后进一步改善
单纯用药疗效有限,未来多要联合治疗心衰
未来慢性心衰治疗可能推荐的药物:
改善预后药物:β受体阻滞剂、LCZ696、醛固酮拮抗剂、伊伐布雷定、中药如芪苈强心胶囊
改善症状的药物:利尿剂、地高辛
其他有效药物:ACEI/ARB、肼屈嗪+硝酸异山梨酯
未来慢性收缩性心衰的基本方案:
β受体阻滞剂、LCZ696、醛固酮拮抗剂组成的“金三角”。
最后,黄院长总结到:新理念正在成形,新的研究正在进行,新的机会正在前头,美好的前景值得我们期待!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










感谢怎么好的学习资源。
54
值得学习
59
牛,学习了。
111
总是有多种矛盾的
100
未来的方向,不知道是否会进一步发展
121
未来的方向,不知道是否会进一步发展
104
未来的方向,不知道是否会进一步发展
83
未来的方向,不知道是否会进一步发展
71
未来的方向,不知道是否会进一步发展
88
未来的方向,不知道是否会进一步发展
115