Crit Care:脓毒性休克患者静脉注射维生素C治疗的效果分析
2022-01-29 MedSci原创 MedSci原创
该初步研究表明静脉注射维生素C并没有显著降低血管升压剂的剂量或持续时间。考虑到干预时间、剂量和持续时间以及试验地点的潜在影响,需要进一步的研究来提供更明确的证据。
脓毒性休克患者静脉注射维生素C可能对血管升压药的需求有一定的影响。

近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,研究人员旨在明确静脉注射维生素C对感染性休克患者血管升压药需求和其他结局的影响。
这是一项在40名感染性休克患者中进行的双盲、随机安慰剂对照试验,受试者随机(1:1)接受静脉注射维生素C(剂量为25mg/kg体重/h)或安慰剂(静脉注射5%葡萄糖)治疗,最长治疗时间96小时,或直至死亡或出院。该研究的主要结局是静脉输注血管升压药的需求(剂量和持续时间),该研究的次要结局包括顺序器官衰竭评估(SOFA)评分、重症监护病房(ICU)和住院时间以及死亡率。此外,研究人员收集了血样以确定维生素C和炎症标志物浓度。
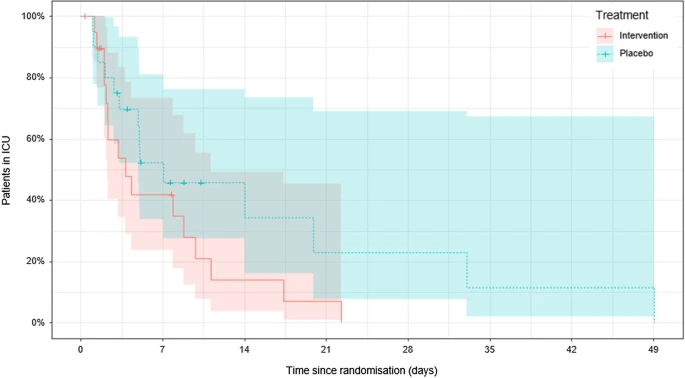
基线时受试者血浆维生素C较低(9.2[4.4-12]µmol/L),干预72小时后增加到408(227-560)µmol/L。维生素C组静脉血管升压药输注的平均持续时间为48(95%CI为35-62)小时,安慰剂组为54(95%CI为41-62)小时(p=0.52)。随着时间的推移,两组的血管升压药剂量相当,SOFA评分也相当(p>0.05)。干预组的中位ICU停留时间为3.8(2.2-9.8)天,而安慰剂组为7.1(3.1-20)天(p=0.12)。维生素C组的中位住院时间为18(11-35)天,而安慰剂组为22(10-52)天(p=0.65)。两组的死亡率相当(p>0.05)。在炎症标志物中,相对于安慰剂组,维生素C组的中性粒细胞计数在72小时内升高(p=0.01)。C-反应蛋白和髓过氧化物酶浓度在基线时升高,但两组随时间推移仍然相当(p>0.05)。
由此可见,该初步研究表明静脉注射维生素C并没有显著降低血管升压剂的剂量或持续时间。考虑到干预时间、剂量和持续时间以及试验地点的潜在影响,需要进一步的研究来提供更明确的证据。
原始出处:
Patrice Rosengrave,et al.Intravenous vitamin C administration to patients with septic shock: a pilot randomised controlled trial.Critical Care.2022.https://ccforum.biomedcentral.com/articles/10.1186/s13054-022-03900-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#脓毒性休克#
22
#静脉#
42
#效果分析#
45
#脓毒性#
43
#脓毒性休克#
50
#静脉注射#
59