JACC:他汀类药物可降低无心血管病史患者中风与心梗风险
2013-12-18 佚名 丁香园
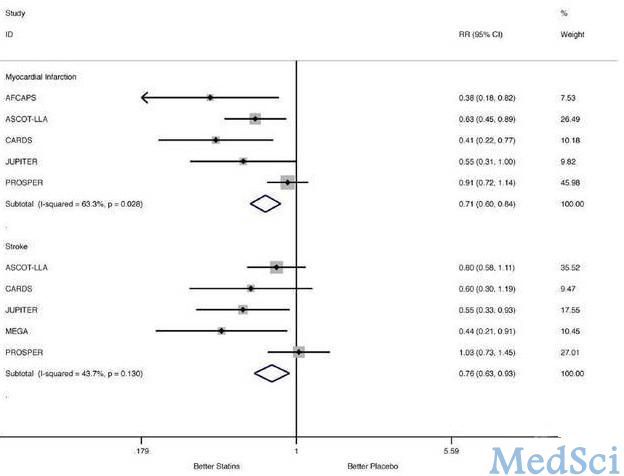
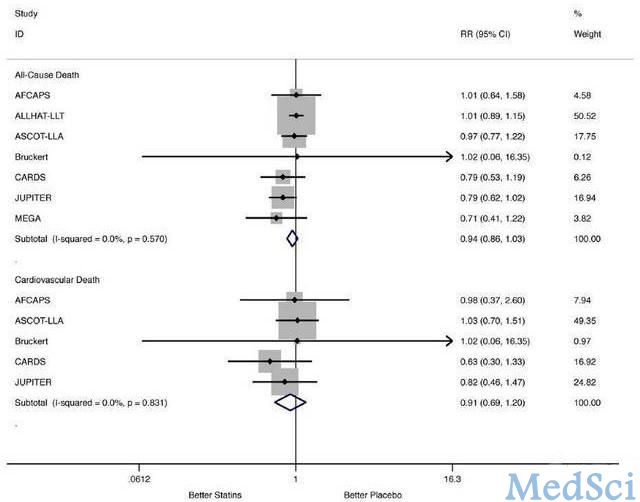
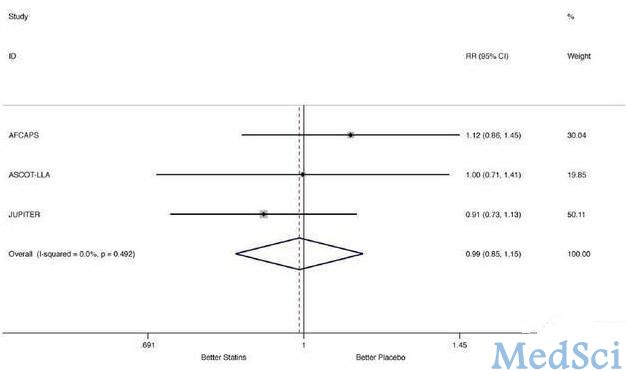
森林图:心肌梗塞与中风在他汀类药物和安慰剂组中风险比较 非心源性死亡和心源性死亡在他汀类药物和安慰剂组中风险比较 新生肿瘤在他汀类药物和安慰剂组中风险比较 研究要点: 1.与年轻人相比,81%的心血管源性死亡在65岁以上老年群体中。目前的指南推荐,既往有心血管病史的老年患者(年龄不低于65岁)应使用他汀类药物,而对于既往无心血管病史的老年人来说,临床指南并不支持使用
森林图:心肌梗塞与中风在他汀类药物和安慰剂组中风险比较
非心源性死亡和心源性死亡在他汀类药物和安慰剂组中风险比较
新生肿瘤在他汀类药物和安慰剂组中风险比较
研究要点:
1.与年轻人相比,81%的心血管源性死亡在65岁以上老年群体中。目前的指南推荐,既往有心血管病史的老年患者(年龄不低于65岁)应使用他汀类药物,而对于既往无心血管病史的老年人来说,临床指南并不支持使用他汀类药物。因此,研究人员进行此项研究,旨在评估他汀类药物能否降低非血管源性死亡与心血管事件风险。【原文下载】
2.这项研究表明,既往无心血管病史的老年高危心血管人群,使用他汀类药物治疗可明显降低心肌梗塞与中风发生风险。因此,研究人员认为他汀类药物对于无心血管病史的老年高危人群同样有效。
与年轻人相比,81%的心血管源性死亡在65岁以上老年群体中。目前的指南推荐,既往有心血管病史的老年患者(年龄不低于65岁)应使用他汀类药物,而对于既往无心血管病史的老年人来说,临床指南并不支持使用他汀类药物。针对这一问题,来自意大利的Gianluigi Savarese博士等进行了一项研究,旨在评估他汀类药物能否降低非血管源性死亡与心血管事件风险。这项研究表明,既往无心血管病史的老年高危心血管人群,使用他汀类药物治疗可明显降低心肌梗塞与中风发生风险。研究结果发表于2013年12月3日的JACC杂志上。
该研究为Meta分析,研究数据来自于使用他汀类药物的文献,这些文献相关研究均是在既往无心血管病史的老年人(≥65岁)中进行。此外,这些研究完整记录了非心血管源性死亡、心血管源性死亡、心肌梗塞、中风、新生肿瘤等情况的随机对照临床试验。入选的八项临床试验总共纳入24674名患者,其中女性占42.7%,平均年龄为73.0±2.9岁,平均随访时间为3.5±1.5年。
研究结果表明,与安慰剂组相比,使用他汀类药物患者心肌梗塞的风险明显下降39.4%,发生中风的风险明显下降23.8%.不过,他汀类药物治疗组患者在非心血管源性死亡和心血管源性死亡的发生风险上并无明显下降;他汀类药物治疗组新生肿瘤发生风险与安慰剂组也无明显差异。
综上,既往无心血管病史的老年高危心血管人群,使用他汀类药物治疗可明显降低心肌梗塞与中风发生风险,但在短期内并不显著延长生存时间。
原文出处:
Savarese G, Gotto AM Jr, Paolillo S, D'Amore C, Losco T, Musella F, Scala O, Marciano C, Ruggiero D, Marsico F, De Luca G, Trimarco B, Perrone-Filardi P.Benefits of statins in elderly subjects without established cardiovascular disease: a meta-analysis.J Am Coll Cardiol. 2013 Dec 3;62(22):2090-9. doi: 10.1016/j.jacc.2013.07.069. 【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#他汀类药#
28
#心梗风险#
35
#JACC#
26
#血管病#
38
#ACC#
33