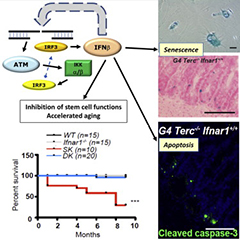
Cell Reports:IFN-beta:早衰恶魔or抗肿瘤先锋?
2015-05-08 佚名 生物谷
长久以来,我们认为机体的衰老与DNA的损伤存在紧密的联系。老年人体内会出现大量的DNA突变事件,同时很多老龄化的症状开始显现。根据小鼠模型,老年小鼠的DNA损伤能够引起基因组的不稳定,影响干细胞的再生能力,从而导致组织的老化与异常。 虽然DNA损伤与细胞老化的联系长久以来深入人心,但其中的分子机制并不清楚,尽管之前有很多研究集中在DNA损伤事件发生后引起的旁分泌效应(paracrine acti
长久以来,我们认为机体的衰老与DNA的损伤存在紧密的联系。老年人体内会出现大量的DNA突变事件,同时很多老龄化的症状开始显现。根据小鼠模型,老年小鼠的DNA损伤能够引起基因组的不稳定,影响干细胞的再生能力,从而导致组织的老化与异常。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
29
#Cell#
30
#BET#
35
#IFN#
31
看看
96