JAHA:糖尿病对稳定胸痛患者评估的影响!
2017-10-31 xing.T MedSci原创
由此可见,稳定的胸痛患者无论有无糖尿病都有相似的临床表现和阻塞性CAD可能性;然而,医生认为糖尿病患者发生阻塞性CAD的可能性更高。需要进一步评估糖尿病对CAD评估的影响。
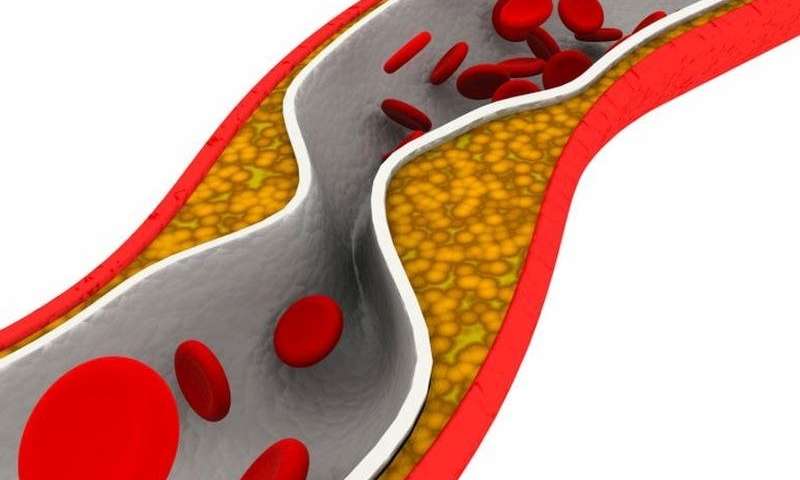
糖尿病对稳定的表现为冠状动脉疾病(CAD)症状的门诊患者临床表现和非侵入性检查(NIT)结果的影响还没有得到很好的描述。近日,心血管疾病领域权威杂志JAHA上针对这一问题发表了一篇研究文章。
该研究招募了10003名糖尿病患者,研究人员对其中8966人进行随机检测,并得到可解释的结果(1908名糖尿病患者,21%)。研究人员采用logistic回归评估症状和NIT结果的差异。
糖尿病患者和无糖尿病患者相比,其年龄(中位数为61岁和60岁)和性别(女性分别为54%和52%)相类似,但是糖尿病患者心血管合并症的负担更大,并无胸痛症状的几率类似(29% vs. 27%)。Diamond-Forrester/冠状动脉手术研究评分预测糖尿病患者与无糖尿病患者发生阻塞性冠心病的可能性相似(低1.8% vs. 2.7%,中间92.3% vs. 92.6%,高5.9% vs. 4.7%)。医生估计的糖尿病患者患阻塞性冠心病的可能性更高(从低到非常低:28.3% vs. 40.1%,中间63.9% vs. 55.9%,高到非常高7.8% vs. 4%)。糖尿病患者(与与无糖尿病患者相比)更可能出现阳性NIT结果(15% vs. 11%;调整后的比值比为1.23;P=0.01)。
由此可见,稳定的胸痛患者无论有无糖尿病都有相似的临床表现和阻塞性CAD可能性;然而,医生认为糖尿病患者发生阻塞性CAD的可能性更高。需要进一步评估糖尿病对CAD评估的影响。
原始出处:
Abhinav Sharma,et al. Impact of Diabetes Mellitus on the Evaluation of Stable Chest Pain Patients: Insights From the PROMISE (Prospective Multicenter Imaging Study for Evaluation of Chest Pain) Trial.JAHA.2017. https://doi.org/10.1161/JAHA.117.007019
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了谢谢作者分享!
72
学习了谢谢作者分享!
86
#AHA#
19
很好的文章.
63