科研助手丨RCT的报告规范——CONSORT声明
2017-11-28 赵俊强 国际护理科学
上一期我们和大家分享了关于RCT研究方案报告的SPIRIT声明,我们明确了在开展一项RCT研究之前,需要参考SPIRIT声明进行严谨规范的科研设计,需要对研究方案进行注册并尝试发表,接下来就是严格按照试验方案开展RCT,并撰写报告(论文)了。但您知道RCT报告(论文撰写)也是有规范的吗?那么接下来小编就和大家具体分享关于RCT报告规范的CONSORT声明。
尽管RCT是评价干预效果的金标准,但是由于研究者水平各异,研究质量也就参差不齐。因此,为了保证研究者撰写清晰、完整和透明的临床研究报告,提高报告质量,也为了帮助读者评判该报告的内外部真实性,CONSORT声明应运而生。
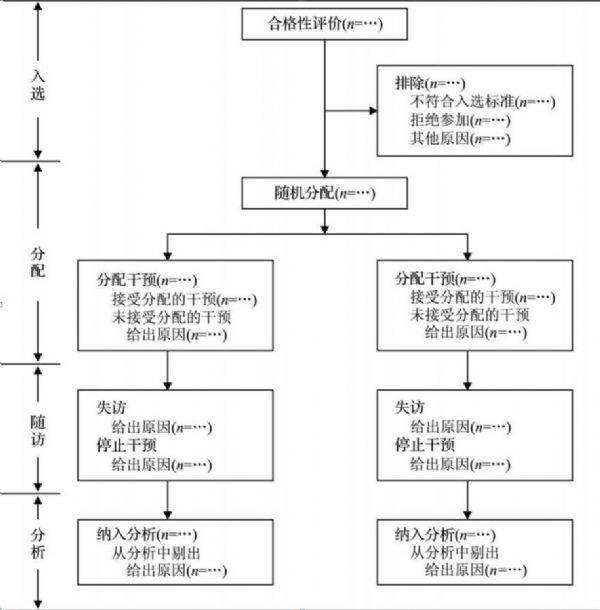
1995年,一个由临床研究者、统计学家、流行病学家和生物医学编辑组成的国际小组制定了“临床试验报告统一标准(Consolidated Standards of Reporting Trials,CONSORT)声明”,并在JAMA上发表,而后在2001年和2010年分别进行了修订和更新,最终形成了包括1张25项条目的清单(表1)和1张流程图(图1)。另外该工作组还提供了CONSORT 2010 说明与详述文本,该文本解释了清单中每一条目的纳入理由,并提供了与方法学相关的背景资料,并以实例加以说明。该声明可为各种随机对照试验提供指导,但主要针对最常用的两组平行随机对照试验。
表1 2010版CONSORT声明
图1 2010版CONSORT声明
此外CONSORT小组还提供了其他类型的报告声明,如群组随机试验(clusterrandomizedtrials)CONSORT扩展版,非劣效性和等效性随机试验(non-inferiority and equivalence randomized trials)CONSORT扩展版,针对中医药的CONSORT声明(CONSORT for Traditional Chinese Medicine),针刺临床试验的CONSORT声明(Reporting Interventions in Clinical Trials of Acupuncture, STRICTA),草药干预临床试验的CONSORT声明和非药物治疗干预的CONSORT声明等。目前,国际上400多本期刊和3个主流的编辑组织(国际医学期刊编辑委员会(ICMJE)、科学编辑委员会(CSE)和世界医学编辑联合会(WAME))对CONSORT声明都给予了官方支持。
目前护理领域的RCT报告与CONSORT声明还存在一定的差距,尤其是方法部分的随机分配隐藏和盲法方面还有待提高[1]。研究表明,与应用了充分分配隐藏的随机对照试验相比,应用不充分或者不清楚是否应用分配隐藏的试验至少将疗效放大了40%[2],如果RCT 的论文没有做到双盲,其疗效也会膨胀35%~40%,以致过度评估阳性疗效而误导临床工作人员[3]。可见随机分配隐藏和盲法对于RCT的内部真实性至关重要。
下面我们结合实例——文献漫游第8期的RCT(公众号内回复“Shelly-Anne原文”可获取原文),来评判一下这篇文章是否严格按照CONSORT声明进行了撰写。CONSORT包括文题和摘要、引言、方法、结果、讨论和其他信息几个主要部分,由于篇幅所限,这一期我们不对方法部分进行分析,在下一期的RCT质量评价工具中,我们再详细解读RCT的方法学质量。(以下均为个人拙见,欢迎批评指正)
1文题和摘要
文题中提到“A Blinded, Randomized Controlled Trial(盲法随机对照试验)”,采用了结构化的摘要清晰明确地表明了研究目的,方法部分描述了目标人群,研究设计(随机、盲法、分配隐藏、双臂试验、随访时间)等关键信息。描述了主要结局和相关讨论。不足之处:缺乏具体的随机方法;受试对象所处环境(setting);结果缺乏关键数据;研究方案的注册号;本研究的经费支助来源等。
2引言
报告了耳鸣的流行病学特征,目前的耳鸣治疗方法存在的局限性,引出本篇RCT研究的必要性。简单明了。紧接着提出自己的研究假说:The present study aims to investigate the effectiveness of this personalized music therapy on chronic, subjective tinnitus among adults(本研究旨在探讨这种个性化的音乐治疗对慢性成人主观性耳鸣的有效性)。如果在这部分报告耳鸣的严重危害会更加有助于解释此项研究的意义。
3方法
此部分在RCT质量评价部分具体论述。
4结果
(1)受试者流程图: 使用流程图表示了从入选,到随机分组,随访和分析全过程,报告了每组随机分配的研究对象数,接受治疗的对象数,完成试验以及进行了主要结局指标分析的例数。
(2)没有具体说明招募和随访的具体时间。
(3)结果部分用了两个表格来说明基线人口统计学资料和临床特征(如:性别、耳鸣类型、治疗史、年龄、耳鸣程度和心理焦虑程度等)。
(4)分析的人数,这部分实际上是了解是否进行了意向性分析(分组后不论出现了什么情况,都要按照随机分配的最初的全部受试者进行统计分析)。本研究中3个月、6个月和12个月纳入分析的人数均为排除失访脱落的人数,未采用意向性分析的方法。而作者在文章讨论的局限性部分也进行了说明,由于此项研究12个月的失访率大于30%,补充大量的缺失数据,会高估或低估治疗效果,所以未使用意向性分析。
(5)描述了主要结局指标——耳鸣困扰(使用量表THI进行评价),以及一些次要结局指标——焦虑和抑郁水平等。报告了效应量和p值,未见95%可信区间。
(6)运用了Bonferroni校正分析的方法。
5讨论
(1)局限性方面,作者讨论了4点局限性分别关于小样本量影响结果的可靠性,没有使用意向性分析,通过自我报告判断患者的依从性存在局限,和改变音乐频谱算法的自身局限性。
(2)针对每一条局限性,作者给予了解释,并提醒读者谨慎对待结果的解读和可推广性。
6其他信息
在利益冲突中指出该研究得到了Sound Options耳鸣治疗公司的资助。但未进行方案的注册。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













还得是中文
13
#报告规范#
49
#CONSORT#
49
#CONSORT#
40
学习了.谢谢.
72
学习了新知识
69
学习了新知识
58
学习了新知识
50