Sci Transl Med:新型近交小鼠模型,开辟了丁肝治疗的新道路
2018-07-01 胖胖同学 iNature
2018年6月27日,普林斯顿大学、康奈尔大学、纽约大学等众多研究人员在Science Translational Medicine上发表了题为“Preclinical assessment of antiviral combination therapy in a genetically humanized mouse model for hepatitis delta virus infect
2018年6月27日,普林斯顿大学、康奈尔大学、纽约大学等众多研究人员在Science Translational Medicine上发表了题为“Preclinical assessment of antiviral combination therapy in a genetically humanized mouse model for hepatitis delta virus infection”的研究论文。在这里,研究人员创建了HDV的转基因(tg)小鼠模型,其表达HBV和HDV的功能性受体,即人牛磺胆酸钠共转运肽NTCP。研究进一步证明myrcludex B和lonafarnib的单一和双重治疗有效地抑制了病毒血症但在测试剂量下未能治愈HDV感染。这种对HDV具有遗传易感性的小动物模型为研究病毒发病机制和免疫反应以及测试新型HDV治疗剂开启了机会。
慢性丁型肝炎(CHD)是由丁型肝炎病毒(HBV)引起的,1977年首次被描述为一种独特的血液传播型肝炎。 HDV是一种1679个核苷酸的包膜负义RNA卫星病毒,也是delta病毒属的唯一成员。小的HDV环状基因组只有1.7kb左右的长度,并且通过广泛的分子内碱基配对来稳定。HDV编码一个单一的开放阅读框架编码的抗原(HDAg),其存在两种异构体:small和large HDAg。因为HDV需要HBV表面抗原(HBsAgs)来包装病毒颗粒,因此依赖于HBV的存在,它被认为是亚病毒卫星。因此,HDV进入肝细胞的早期步骤与HBV相同。
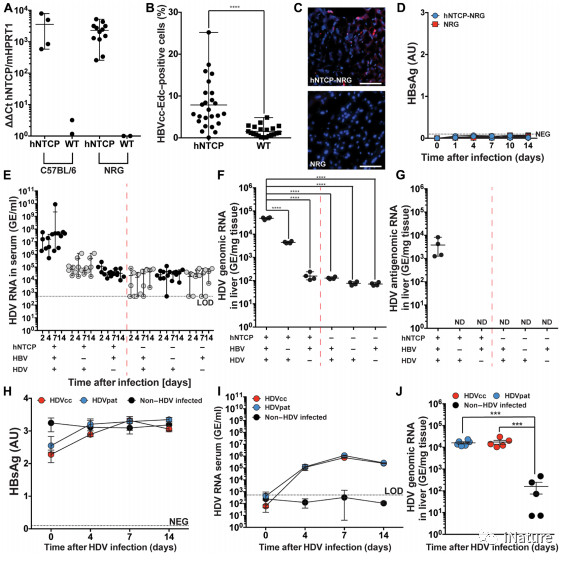
hNTCP / BAC-NRG小鼠促进HBVcc和HDVcc的摄取
一旦在肝细胞内,HDAg-L上的核定位信号触发HDV核衣壳易位至核,其中病毒基因组被复制。 HDV基因组的小尺寸导致病毒依赖于宿主酶,包括细胞RNA聚合酶,以成功复制。传入的RNA可作为比病毒基因组大小更长的转录物的模板。这种多聚体线性RNA含有至少两个反基因组核糖核酸的拷贝,在自我切割后释放单位长度的线性RNA。在类似的中间步骤之后,抗基因组RNA被环化并形成新的基因组RNA的模板。
hNTCP / BAC-NRG小鼠中持续性HDV感染的表征
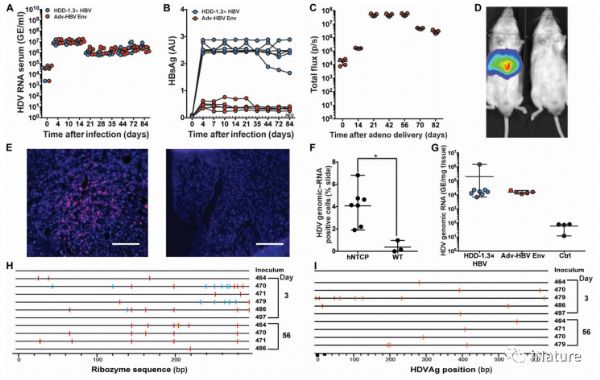
由丁肝病毒(HDV)引起的慢性乙型肝炎是最严重的病毒性肝炎。全球至少2000万乙型肝炎病毒(HBV)感染患者。 HDV / HBV共同或超重感染是肝癌发生的主要驱动因素。抗病毒治疗仅适用于HBV,只能抑制但不能治愈感染。由于缺乏合适的小动物模型,阻碍了更有效疗法的开发。在这里,研究人员创建了HDV的转基因(tg)小鼠模型,其表达HBV和HDV的功能性受体,即人牛磺胆酸钠共转运肽NTCP。 HBV和HDV都以糖蛋白依赖的方式进入这些小鼠的肝细胞,但是一个或多个延伸区阻止了HBV的复制。
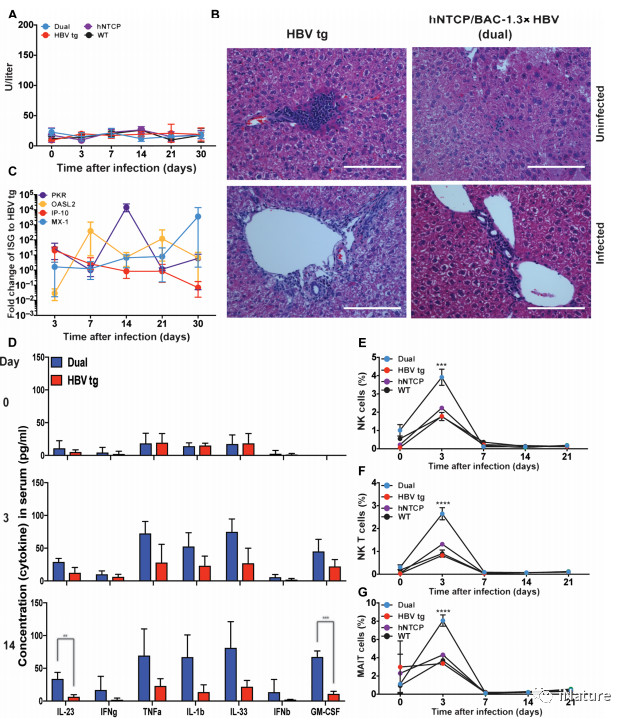
HDV攻击的hNTCP / BAC / 1.3×HBV tg动物的组织病理学特征
相反,HDV持续感染表达HBV包膜的hNTCP tg小鼠,与包装和传播的HBV表面抗原(HBsAg)对HDV的依赖性一致。在缺乏功能性B,T和自然杀伤细胞的免疫缺陷小鼠中,病毒血症持续至少80天,但在免疫活性动物的14天内消失,表明淋巴细胞对于控制HDV感染是关键的。尽管急性HDV感染在该模型中不引起明显的肝损伤,但诱导了细胞内在和细胞固有免疫应答。研究进一步证明myrcludex B和lonafarnib的单一和双重治疗有效地抑制了病毒血症但在测试剂量下未能治愈HDV感染。这种对HDV具有遗传易感性的小动物模型为研究病毒发病机制和免疫反应以及测试新型HDV治疗剂开启了机会。
原始出处:
Benjamin Y. Winer,et al.Preclinical assessment of antiviral combination therapy in a genetically humanized mouse model for hepatitis delta virus infection.Sci Transl Med.27 Jun 2018:Vol. 10, Issue 447, eaap9328
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#TRA#
29
#Transl#
24
#小鼠模型#
38
#Med#
24
学习了!!!!
49