冠状动脉斑块需要治疗吗?
2018-06-05 郭艺芳 郭艺芳心前沿
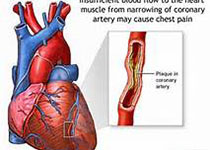
患者,男性,59岁,因间断胸闷在当地医院就诊。查心电图未见异常,LDL-C为3.1mmol/L,冠脉CT示右冠脉与左回旋支有两处斑块形成,伴30-40%的轻度狭窄。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#冠状动脉斑块#
35
#斑块#
30
学习谢谢分享
57
谢谢分享.学习了
60
学习.谢谢分享!
57
学习了谢谢分享!!
51
学习学习再学习
44