PNAS:机械挤压作用促进肿瘤转移
2012-01-06 MedSci原创 MedSci原创
(图片来源:PNAS) 麻省理工学院的Janet M. Tse等近日在《美国国家科学院院刊》(Proceedings of the National Academy of Sciences)发表论文称,机械挤压作用或可促进肿瘤细胞转移。 肿瘤细胞在体内进行不受机体控制的增殖分裂,当其分裂数量到达一定程度后,肿瘤细胞便受到有限的空间带来的挤压。为了研究这种挤压作用对肿瘤细胞的影响,Janet T
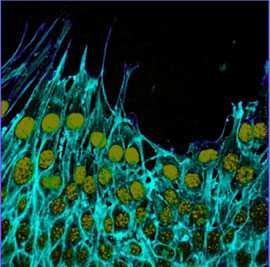
(图片来源:PNAS)
麻省理工学院的Janet M. Tse等近日在《美国国家科学院院刊》(Proceedings of the National Academy of Sciences)发表论文称,机械挤压作用或可促进肿瘤细胞转移。
肿瘤细胞在体内进行不受机体控制的增殖分裂,当其分裂数量到达一定程度后,肿瘤细胞便受到有限的空间带来的挤压。为了研究这种挤压作用对肿瘤细胞的影响,Janet Tse等将乳腺上皮细胞置于一层膜表面,并使用活塞对其进行挤压。
研究者发现,挤压作用可通过刺激细胞层边缘中首先转移的"领头羊"细胞的形成,从而促进乳腺癌细胞的迁移。
"领头羊"细胞可在转移过程中在保持与拖尾细胞保持联系的同时,扩大向迁移方向的突出。
此外,挤压作用可诱导肿瘤细胞分泌一种称为纤维连接蛋白的蛋白质,该蛋白质可通过增强细胞与细胞间和细胞与膜表面间的粘连,从而促进肿瘤细胞的迁移和"领头羊"细胞的形成。
研究者指出,高度侵袭性肿瘤细胞通常受到挤压作用的影响,这或许是由于这些细胞已经随时准备好去改变这种受挤压的环境了。
作者称,肿瘤在生长过程中受到的挤压作用可通过刺激"领头羊"细胞的形成而发生迁移,造成肿瘤转移。机械挤压作用机制为阻止肿瘤迁移和浸润提供了一个新的靶点。(生物谷bioon.com)
Mechanical compression drives cancer cells toward invasive phenotype
Janet M. Tse, Gang Cheng, James A. Tyrrell,Sarah A. Wilcox-Adelman, Yves Boucher, Rakesh K. Jain, and Lance L. Munn.
Uncontrolled growth in a confined space generates mechanical compressive stress within tumors, but little is known about how such stress affects tumor cell behavior. Here we show that compressive stress stimulates migration of mammary carcinoma cells. The enhanced migration is accomplished by a subset of "leader cells" that extend filopodia at the leading edge of the cell sheet. Formation of these leader cells is dependent on cell microorganization and is enhanced by compressive stress. Accompanied by fibronectin deposition and stronger cell-matrix adhesion, the transition to leader-cell phenotype results in stabilization of persistent actomyosin-independent cell extensions and coordinated migration. Our results suggest that compressive stress accumulated during tumor growth can enable coordinated migration of cancer cells by stimulating formation of leader cells and enhancing cell-substrate adhesion. This novel mechanism represents a potential target for the prevention of cancer cell migration and invasion.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#PNAS#
0
#肿瘤转移#
36