乳腺癌亚型与脑转移的发生率、放疗情况和生存期关系如何?JAMA Netw Open发表结果一一解答
2022-09-05 MedSci原创 MedSci原创
JAMA Netw Open:加拿大安大略省脑转移发生率与乳腺癌亚型的相关性分析
脑转移瘤(BRM)是乳腺癌女性发病和死亡的主要原因。患有转移性ERBB2(以前称为HER2)阳性和三阴性乳腺癌(TNBC)的女性具有特别高的发生颅内疾病的倾向;事实上,这些女性中有超过三分之一的人在其一生中发展BRM。乳腺癌BRM患者的主要治疗方法仍然是局部治疗。

尽管有症状的 BRM 对患者和医疗保健系统造成很大负担,但目前的指南不建议使用神经影像学检查来常规筛查早期或转移性乳腺癌 (MBC) 女性的 BRM。然而,缺乏适当的数据来为临床试验或筛查MBC患者BRM的政策提供信息。因此,本研究旨在探索新发MBC患者BRM的累积发病率。
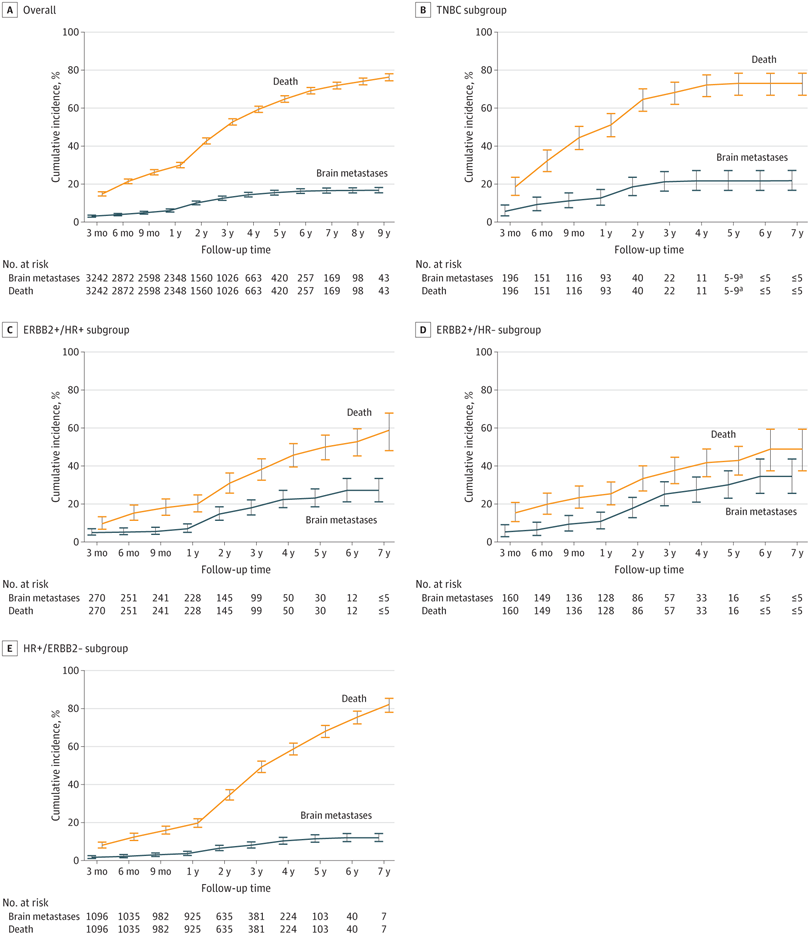
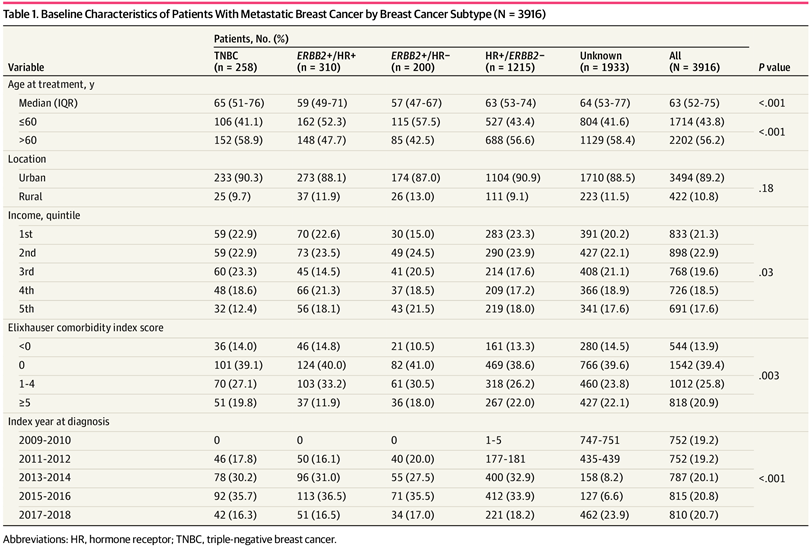
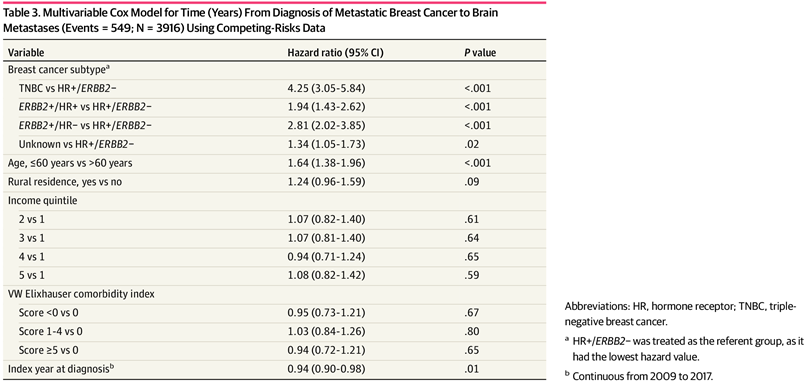
在这项基于人群的队列研究中,加拿大安大略省的人口健康管理数据库在ICES举行,用于识别2009年-2018年期间被诊断为首发MBC的患者。鉴于ICES中不存在BRM代码,研究人员分析了BRM放疗的发生率。中位(IQR)随访时间为19.3(6.2-39.5)个月。最终纳入3916名被确定为首发MBC患者。放疗的累积发生率考虑了竞争性的死亡风险,以及从 MBC 诊断到脑部放疗的时间。对事件发生时间终点执行了 Kaplan-Meier 分析。逻辑回归用于解释混杂变量。
结果显示,在3916例MBC患者中,1215例(31.0%)为HR阳性/ERBB2(原HER2)阴性癌症,310例(7.9%)为ERBB2阳性/HR阳性,200例(5.1%)为ERBB2阳性/HR阴性癌症,258例(6.6%)为TNBC,其余1933例(49.4%)为乳腺癌亚型未知。诊断时的中位(IQR)年龄为63岁(52-75)。共有549人(14.0%)接受了立体定向放射外科手术或全脑放射治疗乳腺癌BRM。
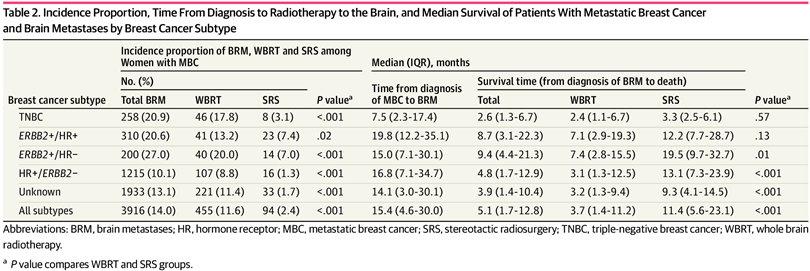
与HR阳性/ERBB2阴性乳腺癌(12.1%)相比,ERBB2阳性/HR阴性乳腺癌(34.7%),ERBB2阳性/HR阳性乳腺癌(28.1%)和三阴性乳腺癌(21.9%)患者的BRM累积发病率更高。
从MBC诊断到脑部放疗的中位(IQR)时间范围为TNBC患者的7.5(2.3-17.4)个月,ERBB2阳性/HR阳性乳腺癌患者的中位(IQR)时间为19.8(12.2-35.1)个月。
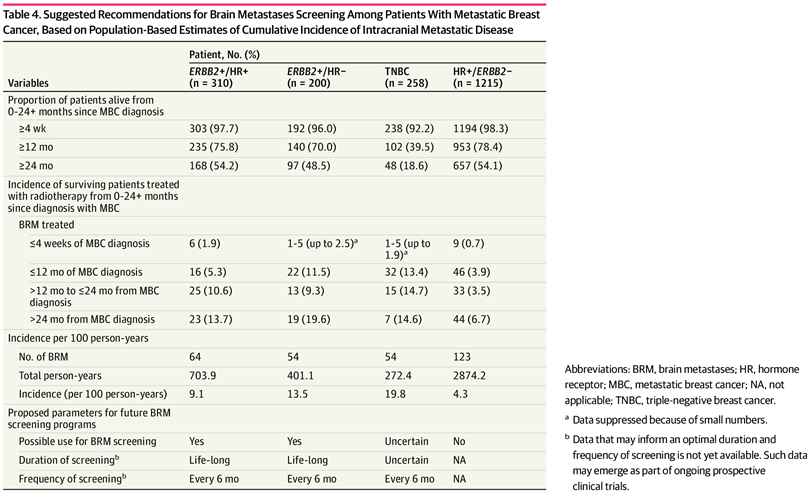
总的来说,BRM 的发生率和发展时间因乳腺癌亚型而异。更好地了解颅内转移性疾病的生物学可能有助于为潜在的筛查计划或预防性干预措施提供信息。
原文来源:
Wang XY, Rosen MN, Chehade R, et al. Analysis of Rates of Brain Metastases and Association With Breast Cancer Subtypes in Ontario, Canada. JAMA Netw Open. 2022;5(8):e2225424. doi:10.1001/jamanetworkopen.2022.25424
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#NET#
43
#发生率#
53
#PE#
29
#生存期#
39
JAMA上文章都是顶级的,谢谢梅斯及时上新
23