
髓鞘-寡核苷酸-糖蛋白(MOG-IgG相关疾病(MOGAD)、aquaporin-4-IgG阳性神经脊髓炎谱系障碍(AQP4-IgG-NMOSD)和多发性硬化症(MS)是中枢神经系统(CNS)不同的炎症性脱髓鞘疾病。尽管有一些重叠的表现,但先前的研究已经强调了这些疾病实体之间的主要差异,特别是关于攻击的严重性和临床过程。
AQP4-IgG-NMOSD和MOGAD的特点是严重发作,通常导致严重的急性残疾(如截瘫、脑病、失明),并经常伴有大脑(最大直径>3厘米)或脊髓(≥3个连续的椎体节段)的大的MRI T2病变,而MS发作通常临床严重程度较轻,并伴有大脑/脊髓MRI的较小病变,尽管一些患者会出现肿瘤性MS病灶。
然而,从长期来看,这些疾病的过程一般不反映最初发作的严重程度。MOGAD患者经常比AQP4-IgG-NMOSD患者有更好的结果,尽管在最低点有类似的严重发作,而继发性进展性残疾基本上是MS所独有的,尽管这种情况下疾病发作较轻。造成这些临床差异的确切原因尚不清楚。这三种疾病的大多数MRI研究都集中在发作性病变的位置和形态或全局性萎缩的测量上,而T2病变的演变却很少被评估。
研究初次发作后不同脱髓鞘病变在MRI上的时间演变可能会提高我们对疾病过程差异的理解,为诊断提供信息,并帮助计划监测疾病活动和治疗的最佳策略。
藉此,Mayo Clinic的Elia Sechi等人,探究了MOGAD、AQP4-IgGNMOSD和MS患者在一次脑或脊髓临床发作后,MRI上脱髓鞘病变的时间演变。
他们回顾性地确定了梅奥诊所的MOGAD、AQP4-IgG-NMOSD或MS患者,以及1)脑部或脊髓炎发作;2)6周内有发作的MRI;3)6个月以上的随访MRI,该区域无间隔性复发。两位神经科医生为每位患者确定有症状的或最大的T2病变(首次病变)。然后由两名对诊断盲的神经放射学专家独立审查MRI,通过共识确定T2病变的解决。在急性期和随访时,手动勾勒出索引T2病变区域,以评估其大小的变化。
结果。我们纳入了156名患者(MOGAD,38;AQP4-IgG-NMOSD,51;MS,67),有172次发作(大脑,81;脊髓炎,91)。
年龄在MOGAD)、AQP4-IgG-NMOSD和MS之间存在差异(P<0.01),女性在AQP4-IgG-NMOSD(41/51[80%])和MS(51/67[76%])组中有差异,但在MOGAD(17/38[45%])的患者中没有。
与AQP4-IgG-NMOSD相比,MOGAD的指标T2病灶完全缓解的频率更高。
与AQP4-IgG-NMOSD相比,所有T2-Lesions的缓解最常发生在MOGAD。MOGAD比AQP4-IgG-NMOSD和MS在后续的轴向脑MRI上的T2病灶面积中位数(范围)减少得更多。
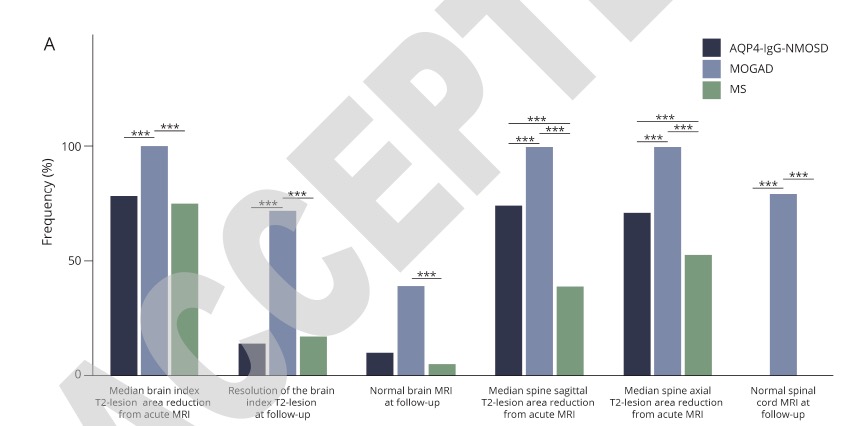 MOGAD和AQP4-IgG-NMOSD在矢状脊柱MRI随访中的大小减少相似(p=0.4),大于MS(23[0-152])(p<0.001)。
MOGAD和AQP4-IgG-NMOSD在矢状脊柱MRI随访中的大小减少相似(p=0.4),大于MS(23[0-152])(p<0.001)。
这个研究的重要意义在于发现了:MOGAD的MRI T2病变比AQP4-IgG-NMOSD和MS更容易完全消散。这对诊断、监测疾病活动和临床试验设计有意义,同时也为中枢神经系统脱髓鞘疾病的发病机制提供了启示。
原文出处:
Sechi E, Krecke KN, Messina SA, Buciuc M, Pittock SJ, Chen JJ, Weinshenker BG, Lopez-Chiriboga AS, Lucchinetti CF, Zalewski NL, Tillema JM, Kunchok A, Monaco S, Morris PP, Fryer JP, Nguyen A, Greenwood T, Syc-Mazurek SB, Keegan BM, Flanagan EP. Comparison of MRI Lesion Evolution in Different Central Nervous System Demyelinating Disorders. Neurology. 2021 Jul 14:10.1212/WNL.0000000000012467. doi: 10.1212/WNL.0000000000012467. Epub ahead of print. PMID: 34261784.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












已读
13
#Neurol#
49
受益匪浅
65
#髓鞘#
44
#脱髓鞘#
42
已读已读已读已读已读,学习学习学习学习,受益匪浅
59
不错,学习了
63