ASCO2021:阿特珠单抗+贝伐珠单抗联合治疗对不可切除肝癌有益
2021-11-25 MedSci原创 MedSci原创
III期IMbrave150试验中位数15.6个月的结果继续支持阿特珠单抗+贝伐珠单抗联合治疗不可切除肝细胞癌患者的一线治疗优于索拉菲尼。
III期IMbrave150试验中位数15.6个月的结果继续支持阿特珠单抗+贝伐珠单抗联合治疗不可切除肝细胞癌患者的一线治疗优于索拉菲尼。
阿特珠单抗+贝伐珠单抗联合vs 索拉菲尼的中位总生存期(OS;19.2个月,13.4个月;分层HR 0.66, 95% CI [0.52, 0.85];p = 0.0009)和独立研究机构评估的中位无进展生存期(PFS) (6.9 vs 4.3个月;分层HR 0.65, 95% CI [0.53, 0.81];p = 0.0001)。
加州大学洛杉矶分校医学博士Richard S. Finn展示了更新后的IMbrave150结果,表示“阿特珠单抗+贝伐珠单抗在晚期肝癌的一线III期研究中有最长的总生存期,证实了这种组合作为以前未治疗的、不可切除的肝癌的标准治疗,”
在IMbrave150的推动下,阿特珠单抗+贝伐珠单抗联合应用于一线不可切除的肝癌患者获得了全球批准,这是基于2020年5月发表的初步分析结果。当时,基于中位随访时间8.6个月,两项共同主要终点均得到满足。阿特珠单抗+贝伐珠单抗的中位OS尚未达到,而索拉非尼的中位OS为13.2个月(HR 0.58, 95% CI [0.42, 0.79];p<0.001)。阿特珠单抗+贝伐珠单抗组的中位无生存期(PFS)为6.8个月,而索拉非尼组为4.3个月(HR 0.59, 95% CI [0.47, 0.76];p <0.001)。
在2021年胃肠癌症研讨会上提出的更新后的IMbrave150结果是很重要的,基于早期Kaplan-Meier生存曲线分离显示阿特珠单抗+贝伐珠单抗的生存获益迅速发生,并持续整个随访期间,尽管大量使用二线和三线治疗,特别是索拉非尼组。52%接受索拉非尼治疗的患者继续接受至少另一条治疗线,而阿特珠单抗+贝伐珠单抗组只有36%的患者这样做。尽管如此,在18个月时,52%的阿特珠单抗+贝伐珠单抗患者存活,而40%的索拉非尼患者存活。
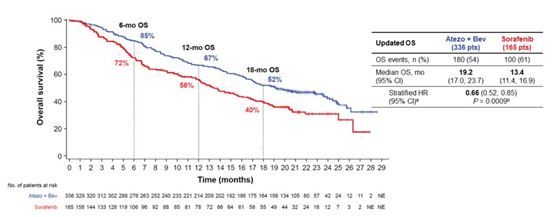
与索拉非尼相比,阿特珠单抗联合贝伐珠单抗观察到的其它有临床意义的益处包括更高的总体缓解率(ORR;30% vs. 11%)和完全缓解(CR)率(8% vs. <1%),以及较长的中位反应持续时间(18.1个月vs. 14.9个月)。当使用改良的RECIST HCC标准评估应答时,这些模式保持稳定,该标准调整了一些指标以更好地反映HCC疾病生物学(ORR: 35% vs. 14%;CR率:12% vs. 3%;中位反应持续时间:16.3个月vs. 12.6个月)。在较长的随访期内,没有出现新的安全信号。阿特珠单抗+贝伐珠单抗组3/4级不良事件的最新发生率为63%,索拉菲尼组为57%。Finn博士指出,联合用药的高发生率可能反映了研究中治疗时间的延长(即,阿特珠单抗中位数为8.4个月,贝伐珠单抗中位数为7.0个月,索拉菲尼中位数为2.8个月)。
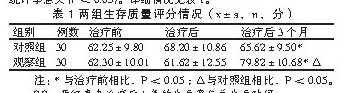
Finn博士还提供了194名中国患者的新亚组数据,这些患者参与了最初的IMbrave150研究或中国特有的扩展队列研究。值得注意的是,在85%的中国人群中,慢性乙型肝炎病毒感染构成了HCC的潜在原因,而在IMbrave150人群中,这一比例为48%。阿特珠单抗+贝伐珠单抗组中国患者的中位OS为24.0个月,索拉菲尼组为11.4个月(分层HR 0.53, 95% CI[0.5, 0.80])。18个月时,56%使用阿特珠单抗+贝伐珠单抗的患者存活,而33%使用索拉非尼的患者存活。
关于IMbrave150的发现是否指向任何生物标记物或临床参数,可以用来选择最有可能对阿特珠单抗+贝伐珠单抗反应的患者。Finn博士等正在寻找生物标志物,但这将是一个挑战。他预计,需要一个基因标记或一组生物标志物来可靠地预测阿特珠单抗+贝伐珠单抗的反应,而不是单一的生物标志物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ASC#
27
#贝伐珠#
25
#联合治疗#
26
#贝伐#
23