紧急降压,舌下含服硝苯地平需谨慎 !
2016-08-25 佚名 药评中心 微信公众号
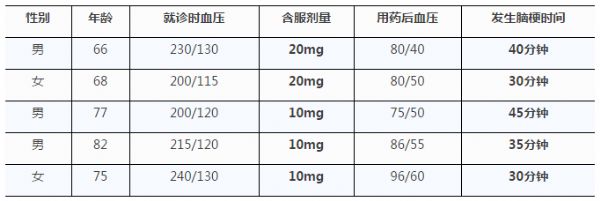
硝苯地平为二氢吡啶类钙拮抗剂,通过舒张外周血管,降低外周阻力,使收缩压和舒张压降低。由于硝苯地平降压效果明显,舌下含服数分钟后起效,作用可持续4~5h,因此曾是门急诊和住院患者治疗高血压急重症的一种常用方法。不少医生认为,舌下含服硝苯地平简单易行,副作用很轻,如脸红、头痛、心动过速等。事实果真如此吗?1、舌下含服硝苯地平的潜在危害美国医学会杂志曾刊登了一篇文章,用很确凿的事实证明:舌下含服硝苯地平
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#硝苯地#
44
文章很好值得关注
85
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
71
学习了,谢谢。
0
#降压#
48
#硝苯地平#
39
#舌下含服#
35
#紧急#
37
深度好文,赞一个!!!
70
学习了,赞一个!!!
68