Cardiovasc Diabetol:恩格列净对2型糖尿病患者右心室参数和功能的影响
2021-11-03 从医路漫漫 MedSci原创
在这项回顾性分析中,恩格列净抑制SGLT2对T2DM和CAD患者的RVMi和RV体积没有影响。恩格列净对左、右心室潜在的差异效应值得进一步研究。
背景:钠-葡萄糖共转运体2 (SGLT2)抑制可减少2型糖尿病(T2DM)心血管事件,并与左心室(LV)质量指数降低相关。其中恩格列净降低了2型糖尿病(T2DM)患者的心血管(CV)死亡率、全因死亡率和心力衰竭(HF)住院时间,并改善了动脉粥样硬化性心血管疾病(ASCVD)。其他SGLT2抑制剂也已经在那些有ASCVD风险或已确诊的ASCVD患者的大型CV结果试验中进行了评估,并显示了类似的结果。最近,证实了恩格列净和达格列净在伴有或不伴有T2 DM的心力衰竭患者中的益处。然而,对右心室重构的影响尚不清楚。因此,本研究的目的是评估SGLT2抑制对T2DM和冠状动脉疾病(CAD)中RV参数和功能的影响。
方法:97例T2DM和CAD患者被随机分配到恩格列净10 mg 组(n = 49)每日1次或安慰剂组(n = 48)。在基线和6个月后进行心脏磁共振成像。盲法评估右心室质量指数(RVMi)、右心室舒张末期和收缩期末期体积指数(RVEDVi, RVESVi)和右心室射血分数(RVEF)。
EMPA-HEART CardioLink-6是一项单中心、双盲、随机、安慰剂对照的IV期试验,研究人员在97名患有T2 DM,6.5%≤HbA1C≤10%的成年患者中进行了试验,入组的患者为接受稳定的降血糖治疗,估计肾小球滤过率≥为60mL/min/1.732,既往有心肌梗死或冠状动脉血管重建病史。在基线时,参与者接受临床和实验室评估,并通过24小时动态血压监测和cMRI进行评估。在标准护理的基础上,纳入的患者按照1:1的比例随机接受6个月每日恩格列嗪10mg或安慰剂治疗。在6个月的随访期间进行了3次临床访问。在基线和6个月时进行超声心动图检查。评估右心室收缩压(RVSP)、三尖瓣反流峰值速度、三尖瓣环形平面收缩偏移(TAPSE)和右心室收缩压(RVSP)。最后一次随访包括再次进行cMRI和24小时动态血压监测。
结果:基线时,恩格列净组RVMi(±SD)(11.8±2.4 g/m2)、RVEF(53.5±4.8%)、RVEDVi(64.3±13.2 mL/m2)和RVESVi(29.9±6.9 mL/m2)均在正常范围内,与安慰剂组相似。超过6个月,恩格列净组与安慰剂组相比没有明显差异,RVMi(−0.11 g / m2, [95% CI 0.81−0.60],p = 0.76), RVEF (0.54%, [95% CI 1.4−2.4],p = 0.58), RVEDVi(−1.2ml/ m2, [95% CI 4.1−1.7],p = 0.41)和RVESVi(−0.81ml/ m2, [95% CI 2.5−0.90],p = 0.35) 。在两组中,RVMi和LVMi从基线到6个月之间没有显著相关性。
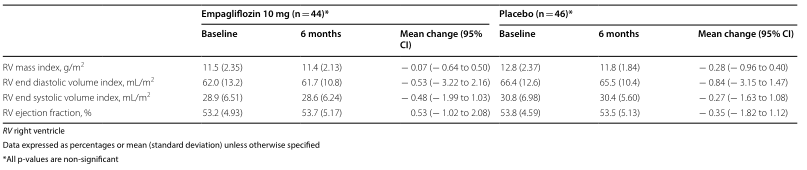
表1 恩格列净和安慰剂治疗6个月后CMRI测量的RV参数的变化
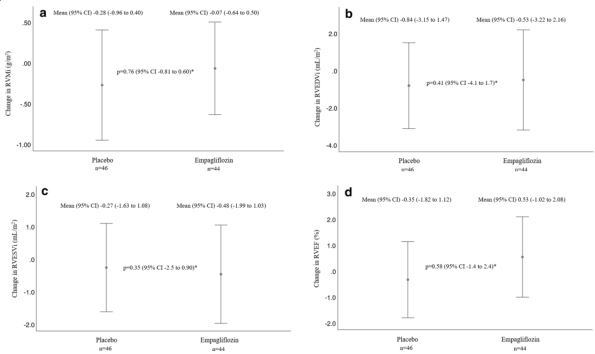
图 (a)与安慰剂相比,恩格列净治疗后6个月RVMi的平均变化。(b)与安慰剂相比,恩格列净治疗后6个月RVEDVi的平均变化。(c)与安慰剂相比,恩格列净治疗后RVESVi的6个月平均变化。(d)与安慰剂相比,恩格列净治疗后RVEF的6个月平均变化。(*)使用ANCOVA对基线进行调整后分析的数据。RVMi,右心室重量指数;RVEDVi,右心室舒张末期容积指数;RVESVi,右心室收缩末期容积指数;RVEF,右心室射血分数。恩格列净组中获得了44人的基线和6个月的数据,安慰剂组中获得了46人的这些数据。RVMi、RVEDVi、RVESVi和RVEF的平均变化以平均值(95%CI)表示,调整后的组间差异以95%CI表示。使用ANCOVA对基准值进行调整来分析数据
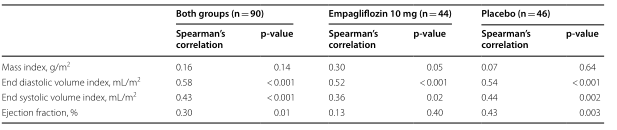
表2 6个月左右左、右心室指数变化关系的Spearman相关系数

表3 右心室指数、生物标志物和血压6个月变化之间的Spearman相关系数
结论:在这项回顾性分析中,恩格列净抑制SGLT2对T2DM和CAD患者的RVMi和RV体积没有影响。恩格列净对左、右心室潜在的差异效应值得进一步研究。
原文出处:
Sarak B, Verma S, David Mazer C,et al.Impact of empagliflozin on right ventricular parameters and function among patients with type 2 diabetes.Cardiovasc Diabetol 2021 Oct 04;20(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIA#
31
#BET#
45
#ASC#
0
#2型糖尿病患者#
32
#糖尿病患者#
28
#右心室#
48