J. Leukocyte. Biol.:揭示IL-8在不同感染位点招募嗜中性粒细胞能力差别
2012-04-14 towersimper 生物谷
基于PDB文件1IL8,利用Pymol构建出的IL-8蛋白三维结构图,图片来自维基共享资源。 来自美国加尔维斯敦市德克萨斯大学医学分校的研究人员发现体内第一道抗感染防御系统利用的制导系统发挥着人们之前未知的新作用。相关研究结果发表在Journal of Leukocyte Biology期刊上。 这项新研究重点研究信号传导分子IL-8的两种存在形式,以及IL-8与糖胺聚糖(glycosamin

基于PDB文件1IL8,利用Pymol构建出的IL-8蛋白三维结构图,图片来自维基共享资源。
来自美国加尔维斯敦市德克萨斯大学医学分校的研究人员发现体内第一道抗感染防御系统利用的制导系统发挥着人们之前未知的新作用。相关研究结果发表在Journal of Leukocyte Biology期刊上。
这项新研究重点研究信号传导分子IL-8的两种存在形式,以及IL-8与糖胺聚糖(glycosaminoglycan, GAG)之间的相互作用。
遭受感染或损伤的组织释放出IL-8来招募杀死细菌和病毒的称作嗜中性粒细胞(neutrophil)的白细胞。IL-8蛋白从感染位点扩散开并把自己锚定在糖胺聚糖上,通过这种方式IL-8提供有助于嗜中性粒细胞找到它们的作用靶标的“路标(signpost)”。
德克萨斯州大学副教授和这篇论文通讯作者Krishna Rajarathnam说,“嗜中性粒细胞是杀伤机器(killing machine),但是它们也是瞎子,所以它们攻击时不分目标,因为要使得它们有效地反抗感染并使得附带组织损伤最小化,它们不得不被精准引导和激活。对这种招募过程的时空控制是非常复杂的,但是我们已获得对这种非常基础性机制的深入了解。”
这一机制基于IL-8存在的单体和二聚体形式。事实上,在感染的发生和消除过程期间,IL-8可能以单体、二聚体或者这两者同时存在。
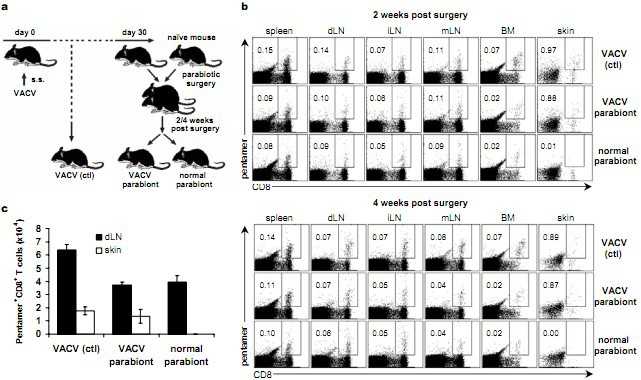
为了研究这种过程如何影响免疫应答,Rajarathnam和他的同事们构建了在自然条件下不存在的两种IL-8形式:一种是由IL-8单体构建而成的,但不能连接而形成二聚体;另一种是由IL-8二聚体构建而成的,但不能切割为单体。他们然后利用构建的IL-8单体和二聚体以及“野生型”(正常的)IL-8执行一系列小鼠实验,他们发现不同浓度的Il-8单体和二聚体明显地影响招募嗜中性粒细胞的强度。
此外,再根据早前的研究,他们确定这些影响的变化由感染位点决定,这就让他们作出结论:IL-8单体和二聚体在身体不同组织与糖胺聚糖发生不同的相互作用。
“我们以前的研究是关于肺部IL-8的,而在这项研究中,我们研究当把IL-8注射进小鼠腹膜(peritoneum)里会发生什么情况”,Rajarathnam说,“在肺部,我们观察到野生型IL-8招募嗜中性粒细胞的能力处于IL-8单体和二聚体单独招募的能力之间,但是在腹膜里,野生型IL- 8实际上招募嗜中性粒细胞的能力更高。这种影响是协同性的,意味着野生型IL-8单体和二聚体协同相互作用从而促进招募嗜中性粒细胞。”
根据Rajarathnam的说法,当在研究复杂的免疫应答时,他就已经能够猜测到这些人们未曾预料到的结果。
“我相信我们发现了一种调控嗜中性粒细胞功能的关键性和基础性的机制。”
“我们未来的研究目标是描述IL-8单体和二聚体功能上的差别以便观察我们是否能够‘控制’包括败血症在内的疾病中发生的炎症扩散(runaway inflammation)和与其相关的嗜中性粒细胞诱导而产生的组织伤害。” (生物谷:towersimper编译)

doi:10.1189/jlb.0511239
PMC:
PMID:
The monomer-dimer equilibrium and glycosaminoglycan interactions of chemokine CXCL8 regulate tissue-specific neutrophil recruitment
Pavani Gangavarapu, Lavanya Rajagopalan, Deepthi Kolli, Antonieta Guerrero-Plata, Roberto P. Garofalo and Krishna Rajarathnam
Chemokines exert their function by binding the GPCR class of receptors on leukocytes and cell surface GAGs in target tissues. Most chemokines reversibly exist as monomers and dimers, but very little is known regarding the molecular mechanisms by which the monomer- dimer equilibrium modulates in vivo function. For the chemokine CXCL8, we recently showed in a mouse lung model that monomers and dimers are active and that the monomer-dimer equilibrium of the WT plays a crucial role in regulating neutrophil recruitment. In this study, we show that monomers and dimers are also active in the mouse peritoneum but that the role of monomer-dimer equilibrium is distinctly different between these tissues and that mutations in GAG-binding residues render CXCL8 less active in the peritoneum but more active in the lung. We propose that tissue-specific differences in chemokine gradient formation, resulting from tissue-specific differences in GAG interactions, are responsible for the observed differences in neutrophil recruitment. Our observation of differential roles played by the CXCL8 monomer-dimer equilibrium and GAG interactions in different tissues is novel and reveals an additional level of complexity of how chemokine dimerization regulates in vivo recruitment.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#嗜中性粒细胞#
27
#Biol#
29
#Bio#
28
#中性粒细胞#
31
#招募#
0
#IL-8#
32