Gut:肝Reptin/RUVBL2通过调控mTORC1和mTORC2信号通路调节糖脂肪代谢
2017-11-23 MedSci MedSci原创
抑制Reptin的表达或活性可能是代谢综合征新的治疗前景。
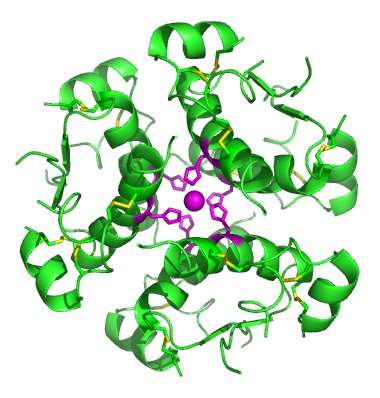
研究背景:Reptin在肝细胞肿瘤中大量表达,临床前研究表明,这可能是一个相关的治疗目标。然而,它在体内的生理和病理生理作用尚不清楚。本研究旨在确定Reptin在哺乳动物成人肝脏中的作用。
研究方法和结果:研究使用肝脏特异的Reptin基因敲除小鼠模型(RepinLKO)。Reptin功能失效后,小鼠体重和脂肪含量降低,低血糖,低血脂。这与mTOR蛋白含量下降有关。研究进一步在原代肝细胞中进行,研究表明,Reptin通过调节ATP酶活性,维持mTOR蛋白水平。出乎意料地是,Reptin功能丧失或者功能被抑制,在mTORC1 and mTORC2信号通路上产生了相反的作用:(1) 强烈抑制肝脏mTORC1活性,肝细胞体积减少,脂肪从头合成减少,胆固醇转录减少 (2) 增强mTORC2活性与葡萄糖转录抑制和肝脏葡萄糖产生减少有关。因此,Reptin在胰岛素抵抗(IR)和非酒精性脂肪肝病中发挥作用。Reptin完全缺失挽救了与IR相关的病理表型,包括葡萄糖耐受、高血糖、高脂血症和肝脂肪变性。
研究结论:抑制Reptin的表达或活性可能是代谢综合征新的治疗前景。
原始出处:
Javary J, Allain-Courtois N, Saucisse N, et al. Liver Reptin/RUVBL2 controls glucose and lipid metabolism with opposite actions on mTORC1 and mTORC2 signalling. Gut, 2017, Oct 26. pii: gutjnl-2017-314208. doi: 10.1136/gutjnl-2017-314208.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











文章很好.学习了
64
#mTORC1#
39
#信号通路#
0
#脂肪代谢#
29
谢谢分享!
55