Hepatol Int:原发性硬化性胆管炎(PSC)患者增加肿瘤发生风险
2021-08-13 yd2015 MedSci原创
该研究表明,与普通人群相比,原发性硬化性胆管炎(PSC)患者患癌症的总体风险增加了近4倍,包括肝胆癌、结直肠癌、胰腺癌以及淋巴瘤。
原发性硬化性胆管炎(PSC)与发生肝胆肿瘤和结肠直肠癌的风险增加有关,但与发生其他肿瘤的风险尚未被探讨。因此。来自瑞士的研究团队开展了相关研究,评估原发性硬化性胆管炎(PSC)患者中发生肠道和肠道外肿瘤的风险。相关结果发表在Hepatology International杂志上。
该研究对瑞典的PSC患者进行了配对的队列研究,每例患者配对多达10例的对照者,对性别、年龄和居住地进行匹配。这些数据是从国家登记册中检索的。从PSC诊断开始随访患者,直到癌症诊断、肝移植、首次移民日期、死亡或2016年12月31日。使用Kaplan Meier方法和Cox回归模型估计癌症风险。
1432名经确诊的PSC患者和14437名对照者进行了研究。大多数PSC患者(69%)为男性。PSC诊断时的中位年龄为31岁。88%的PSC患者发现炎症性肠病(IBD),溃疡性结肠炎(UC)是IBD最常见的亚型(84%)。
平均随访时间为15.9年。1432名PSC患者中318人被诊断为癌症,其中28人被诊断为两种癌症,2人被诊断为三种不同类型的癌症。7例PSC患者同时被诊断为肝胆癌和结直肠癌。PSC患者发生首次癌症的总体风险增加(HR 3.8, 95% CI 3.3 4.3),在PSC诊断后10年、20年和30年,累计发病率分别为12%、27%和45%。这种风险在40岁以上的PSC患者中更明显,但在男性和女性中没有发现差异。
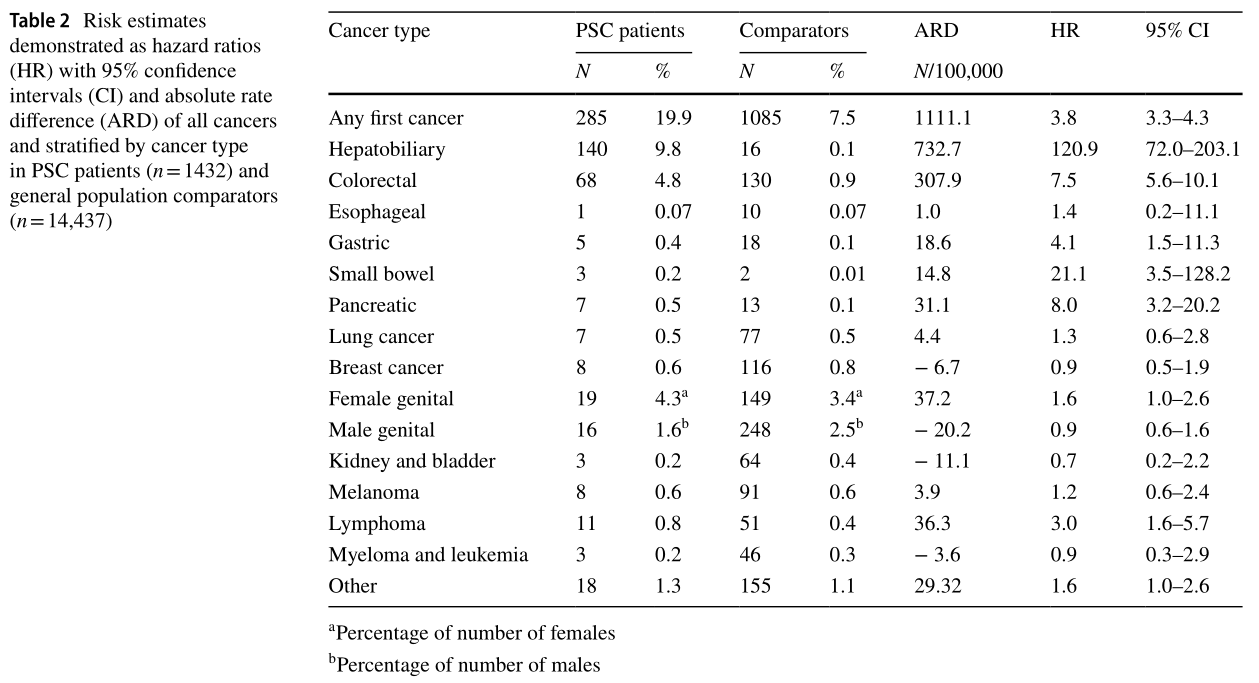
不同肿瘤发生风险
随访期间,10% (n = 140)的PSC患者和0.1% (n = 16)的对照者被诊断为肝胆肿瘤,其中9%的PSC患者和0.1%的对照患者诊断原发肝胆肿瘤。PSC患者肝胆癌的危险度(HR)为120.9 (95% CI 72.0-203.1)。PSC诊断后患者中肝胆肿瘤的10、20和30年累积发病率分别为5%、13%和25%。在患者中风险更明显年龄在40岁以上。
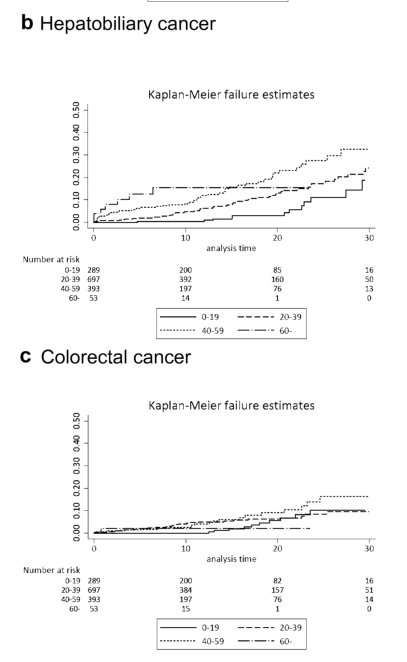
肝胆和结直肠发生风险
PSC患者发生结直肠癌的HR为7.5(95% CI 5.6–10.1),10、20和30年累积发病率分别为3%, 7%, 和11%。PSC患者患胰腺癌[HR 8.0 (95% CI 3.2 20.2)]、胃癌[HR 4.1 (95% CI 1.5 11.3)]和小肠[HR 21.1 (95% CI 3.5 128.2)]的风险也增加。PSC患者发生淋巴瘤的风险增加[HR 3.0 (95% CI 1.6 5.7)]。
综上,该研究表明,与普通人群相比,原发性硬化性胆管炎(PSC)患者患癌症的总体风险增加了近4倍,包括肝胆癌、结直肠癌、胰腺癌以及淋巴瘤。
原始出处:
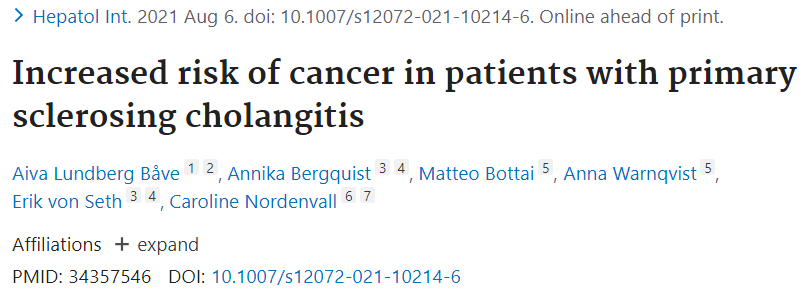
Lundberg Båve A, Bergquist A, Bottai M, et al. Increased risk of cancer in patients with primary sclerosing cholangitis. Hepatol Int. 2021 Aug 6. doi: 10.1007/s12072-021-10214-6. Epub ahead of print. PMID: 34357546.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#原发性#
17
#PSC#
26
#原发性硬化性胆管炎#
66
#EPA#
25
#硬化性#
33
#胆管#
28