Anesthesiology:不可切除胰腺癌患者行神经毁损性内脏神经阻滞与患者疼痛缓解、生存率和生活质量的关系:一项随机对照试验
2021-09-30 “罂粟花”公众号 “罂粟花”公众号
背景
背景
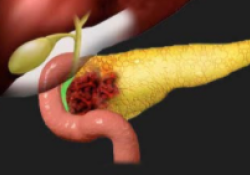
胰腺癌患者的癌痛临床上常用内脏神经毁损治疗。然而,它对胰腺癌患者生存和生活质量的影响仍有争议。作者的主要假设是,使用神经阻滞后,能够更好的缓解癌症疼痛。其次,他们假设使用镇痛剂患者的生存和生活质量会受到影响。
方法
在中国的五个临床试验中心进行这项随机、双盲、平行对照试验。符合条件的中度至重度疼痛患者被随机分配接受无水乙醇组(神经毁损组)或生理盐水内脏神经阻滞组(对照组)。主要结果指标是用视觉模拟量表测量患者的疼痛缓解。记录阿片类药物的消耗量,患者的生存率、生活质量和不良反应。所有临床试验中心采用了统一的镇痛剂的管理方案。对患者进行了8个月或直至患者死亡的随访。
结果
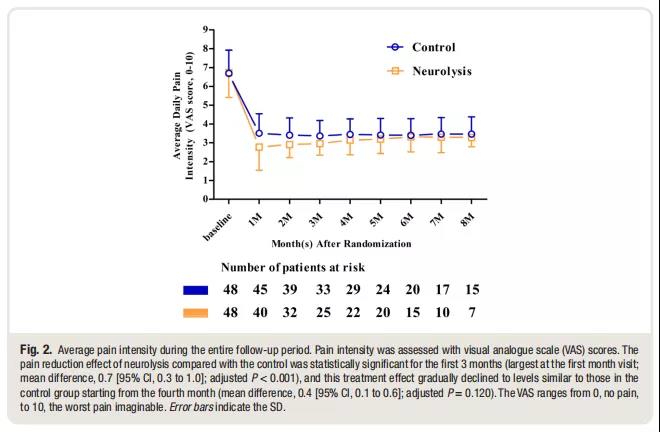
96名患者(每组48人)被纳入分析。与安慰剂注射相比,神经毁损组在头3个月的疼痛缓解程度更高(第一个月最大;均差为0.7[95%CI,0.3至1.0];调整后的P < 0.001)。与安慰剂注射相比,前5个月神经毁损组的阿片类药物消耗量较低(第一个月最大;均差为95.8[95%CI,67.4-124.1];校正后P<0.001)。组间生存率有明显差异(风险比为1.56[95%CI,1.03-2.35];P=0.036)。第四阶段的患者发现神经毁损组生存率明显下降(风险比为1.94[95% CI,1.29-2.93];P = 0.001),但第三阶段的患者没有(风险比,1.08[95% CI,0.59至1.97];P = 0.809)。没有观察到生活质量的差异。




结论
对于不能切除的胰腺癌患者,神经毁损内脏神经治疗似乎是控制疼痛和减少阿片类药物需求的有效选择。
原始出处:
Daosong Dong, Mingfang Zhao, Jingmei Zhang, et al. Neurolytic Splanchnic Nerve Block and Pain Relief, Survival, and Quality of Life in Unresectable Pancreatic Cancer: A Randomized Controlled Trial. Anesthesiology 2021; 135:686–98.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#疼痛缓解#
35
#对照#
41
#对照试验#
37
#EST#
26
#生存率#
34
#随机对照试验#
37
#ESI#
38