BJJ:TKA术后非感染性伤口并发症影响临床疗效
2014-06-04 佚名 丁香园
现较多研究表明关节置换术后伤口并发症如渗出、不愈合、裂开等与术后关节深部感染发生有显著相关性,深部感染影响长期临床疗效同样较多文献报道,而非感染性伤口并发症是否影响术后疗效却鲜有报道。 为了明确需要再次返院处置的术后非感染性伤口并发症是否对术后关节置换疗效有影响,美国Adelani教授回顾性分析全膝置换后发生非感染性伤口并发症患者术后2年临床疗效,结果发表在近期BJJ上。【原文下载】
现较多研究表明关节置换术后伤口并发症如渗出、不愈合、裂开等与术后关节深部感染发生有显著相关性,深部感染影响长期临床疗效同样较多文献报道,而非感染性伤口并发症是否影响术后疗效却鲜有报道。
为了明确需要再次返院处置的术后非感染性伤口并发症是否对术后关节置换疗效有影响,美国Adelani教授回顾性分析全膝置换后发生非感染性伤口并发症患者术后2年临床疗效,结果发表在近期BJJ上。【原文下载】
2005年1月-2010年1月共2221例首次TKA,121例(105例患者)术后90天内因各种原因需再次返院,返院率5.4%。54例因内科并发症返院;67例因手术并发症返院,其中22例ROM受限、17非感染性伤口并发症、12例深部感染、12例凝血障碍、4例VTE。
纳入标准:因非感染性伤口并发症返院患者(伤口渗出、裂开、不愈合、血肿形成、关节积血),至少随访1年,再次返院时关节穿刺、细菌培养阴性排除感染可能。最终15例(伤口渗出4例、裂开5例、不愈合、血肿形成5例、关节积血1例)纳入研究,11例男性、4例女性,平均年龄66岁。
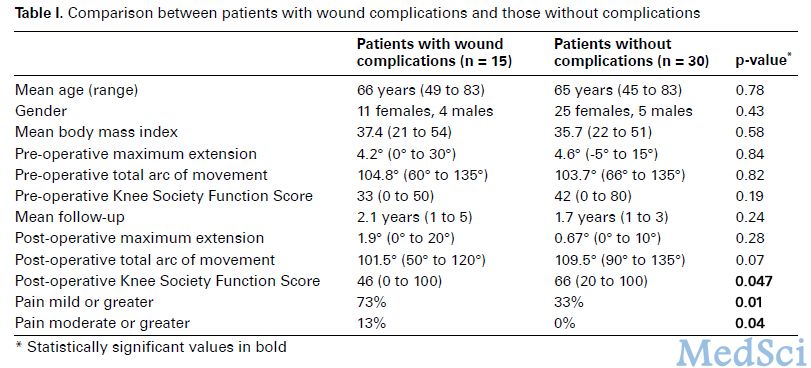
再依据以上15例患者术前基本情况,匹配30例TKA术后90天内未因任何手术并发症返院者为对照组。术前、末次随访评价两组患者ROM、膝关节疼痛评分、膝关节功能评分(KSFS)。
所有患者伤口由实习生或助理缝合,关节囊层1号Vicryl间断缝合,皮下层2-0 Monocryl间断缝合,订书机缝合表皮。常规负压引流,术后1天拔除,术后2周拆线。
15例患者平均返院住院天数5.6天(2-16天)。11例需再次手术干预,其中6例浅层清创术未打开关节腔,2例保留聚乙烯衬垫行关节内清创术,2例术中彻底清洗关节后侧更换衬垫行关节内清创术,1例行腓肠肌皮瓣移植关闭伤口;4例静滴抗生素+局部换药。1例患者返院期间二次清创处置;2例患者二次返院,其中1例因伤口裂开、1例因贫血。
结果:
1、伤口并发症组出现1例因关节活动受限需麻醉下行手法松解,对照组无。
2、末次随访伤口并发症组关节轻度以上疼痛者11例(73%),中度以上疼痛者2例(13%);对照组轻度以上疼痛者10例(33%),中度以上疼痛者无。疼痛方面并发症组明显差于对照组。
3、末次随访平均KSFS伤口并发症组46分明显差于对照组66分。
本次研究中病例数较少,随访年限较短(2年);但作者认为随访年限2年足够因以往研究表明关节置换术后1年关节活动度已稳定;该研究从另一个角度表明不管是否导致术后感染发生,都应该重视术后伤口并发症,告知患者出现伤口并发症时临床疗效将会受影响,当然更大样本研究仍需。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#感染性#
38
#并发#
30
#临床疗效#
37
#TKA#
51
#非感染性#
36