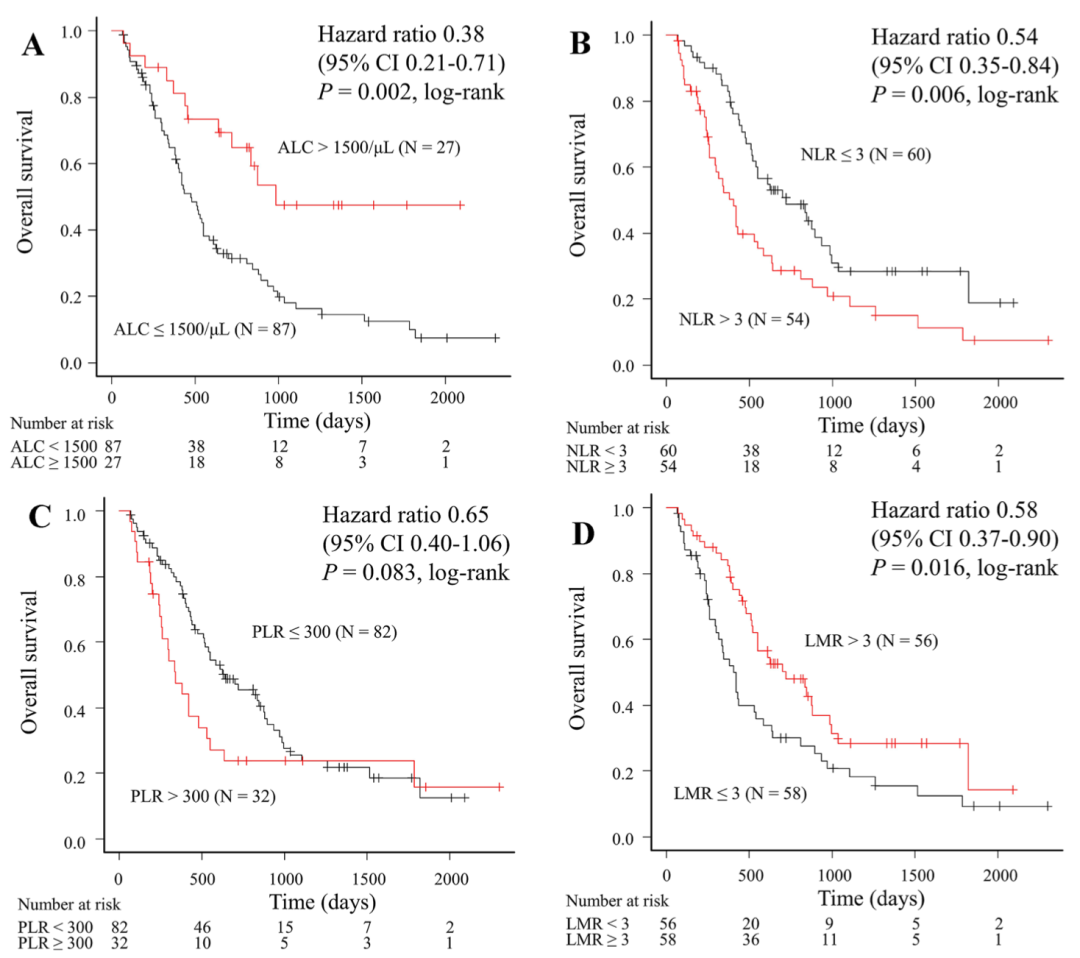
血常规是临床最常用的检查之一,而且血常规结果里还隐藏着和癌症预后相关的秘密。今天小编就带大家来读一读血常规结果,看看里面藏着哪些肿瘤的秘密。 图1 四项血常规指标与至治疗失败时间(TTF)的关系 (A)ALC;(B)NLR;(C)PLR;(D)LMR 图2 四项血常规指标与总生存期(OS)的关系(A)ALC;(B)NLR;(C)PLR;(D)LMR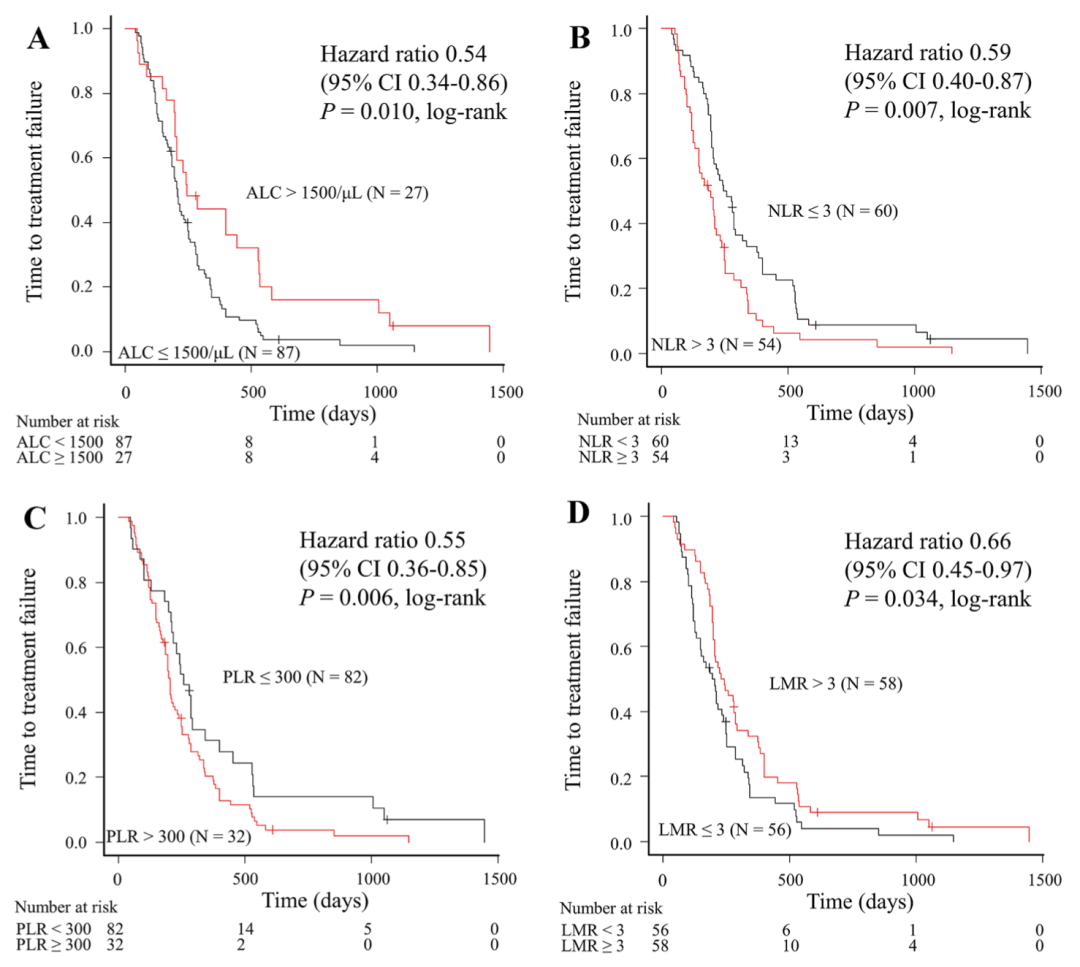
-
NLR值:高NLR组患者5年生存率为19.1%;低NLR组患者5年生存率为47.07%。(差别很大)
-
LMR值:高LMR组患者5年生存率为57%;低LMR组患者5年生存率为26%。(差别很大)
-
PLR值:高PLR组患者5年生存率为40.15%;低PLR组患者5年生存率为42.98%。(几乎无差别)
-
NLR值:高NLR组患者5年生存率为37.8%;低NLR组患者5年生存率为83.1%。(差别很大)
-
LMR值:高LMR组患者5年生存率为73.2%;低LMR组患者5年生存率为50%。(有差别)
-
PLR值:高PLR组患者5年生存率为49.4%;低PLR组患者5年生存率为74.8%。(有差别)
-
NLR值:高NLR组患者中位无进展生存期为19个月;低NLR组患者中位无进展生存期为32个月。(有差别) -
LMR值:高LMR组患者中位无进展生存期为36个月;低LMR组患者中位无进展生存期为19个月。(差别很大) -
PLR值:高LMR组患者中位无进展生存期为22个月;低LMR组患者中位无进展生存期为30个月。(差别不太大)
-
NLR、RDW、PLR:与良性卵巢肿瘤患者相比,卵巢癌患者的这三项值较高;III、IV期宫颈癌患者的这三项值也均高于I和II期宫颈癌患者。
-
LMR:与上面三项值相反,肿瘤恶性程度越高,值反而越低。
-
PLR值较低,与各种实体瘤患者总生存期较长相关。 -
LMR值较高,与各种实体瘤患者总生存期较长相关。 -
NLR值:治疗方案无论是手术、新辅助+手术、放化疗还是不手术的患者,NLR值升高与预后不良有关。
表1 预后影响因素的单因素分析
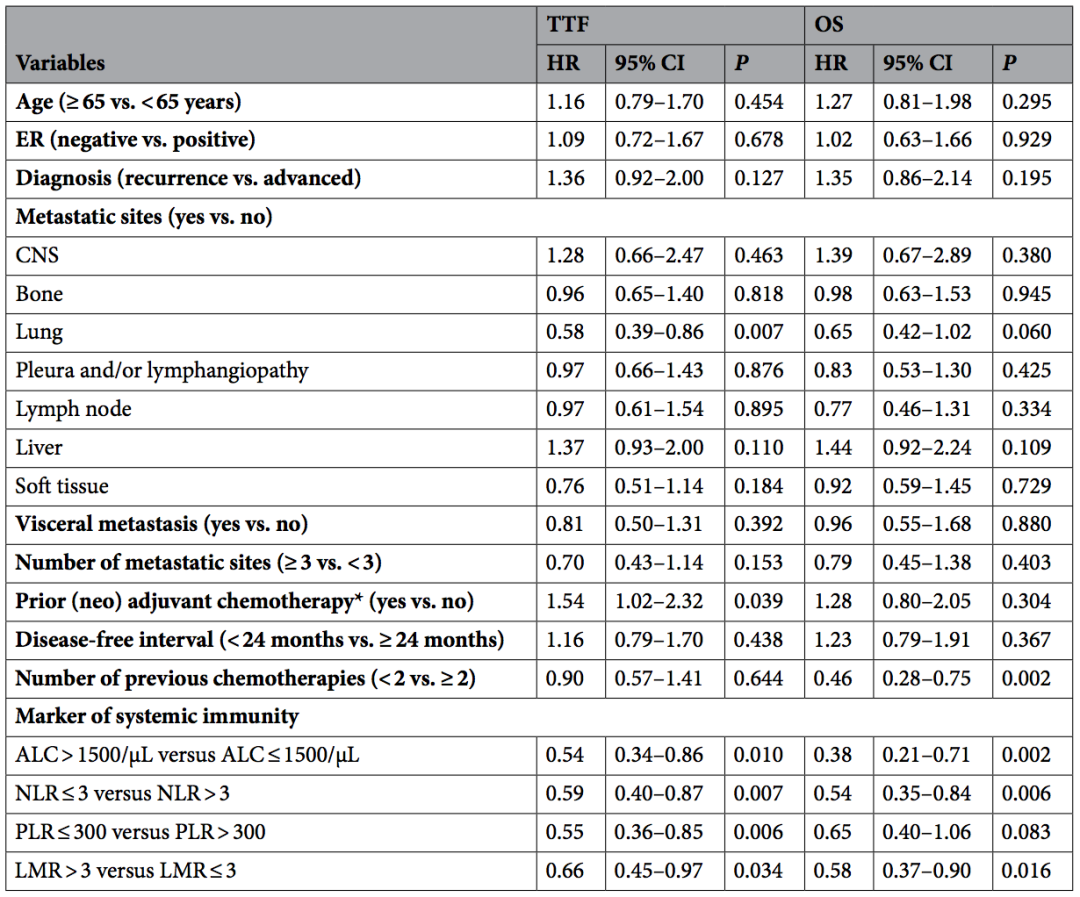
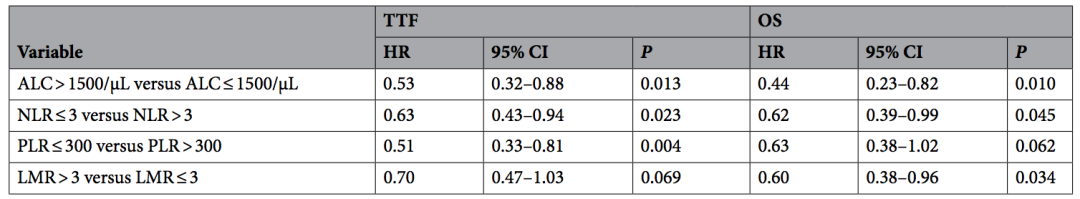
表2 TTF和OS的多因素分析结果
参考文献
Shogo Nakamoto, Masahiko Ikeda, Shinichiro Kubo, et al. Systemic immunity markers associated with lymphocytes predict the survival benefit from paclitaxel plus bevacizumab in HER2 negative advanced breast cancer. Sci Rep. 2021; 11(1): 6328. doi: 10.1038/s41598-021-85948-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习
0
学习了
55
学习了
63
认真学习了
56
学习了,谢谢分享
54
🉑
35