JCO:二甲双胍可以显著改善HER2阳性早期乳腺癌合并糖尿病患者的预后
2017-03-17 Riesling 肿瘤资讯
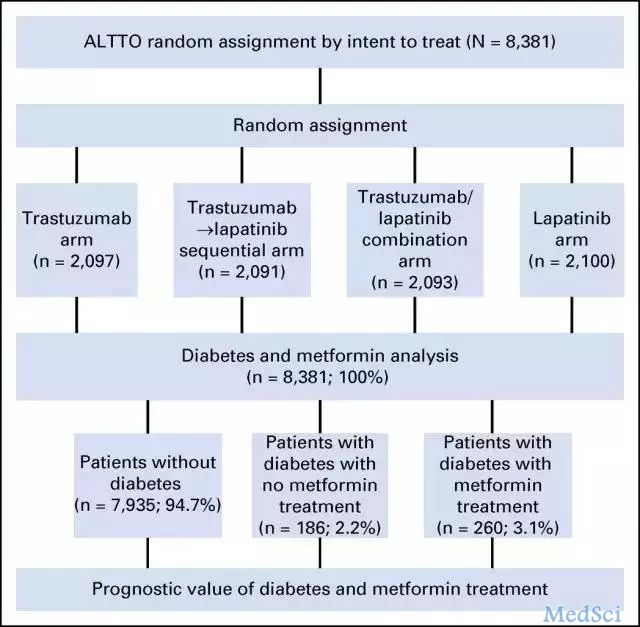
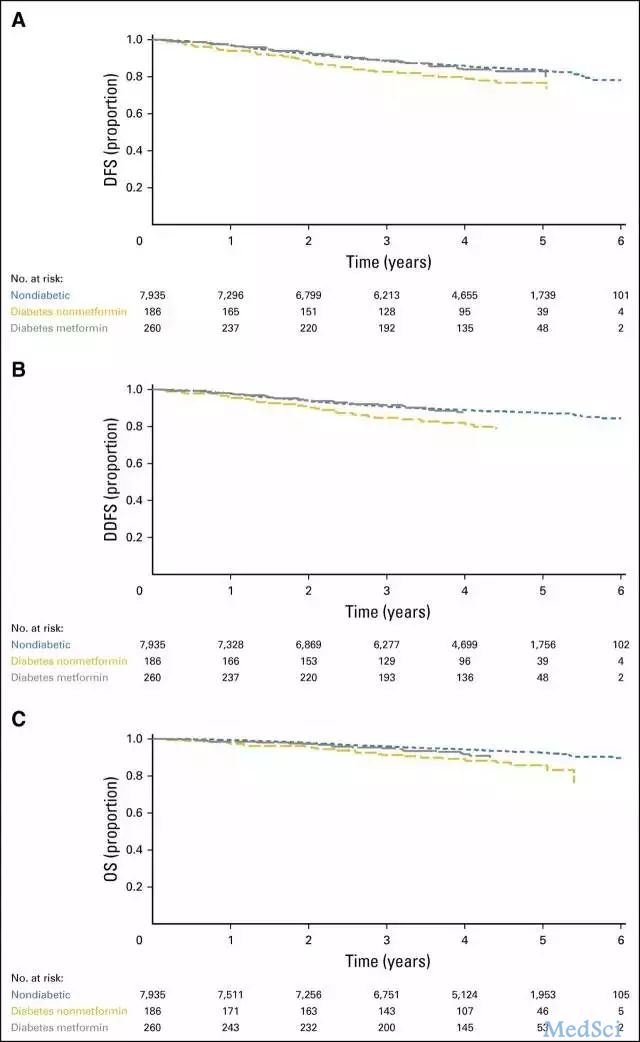
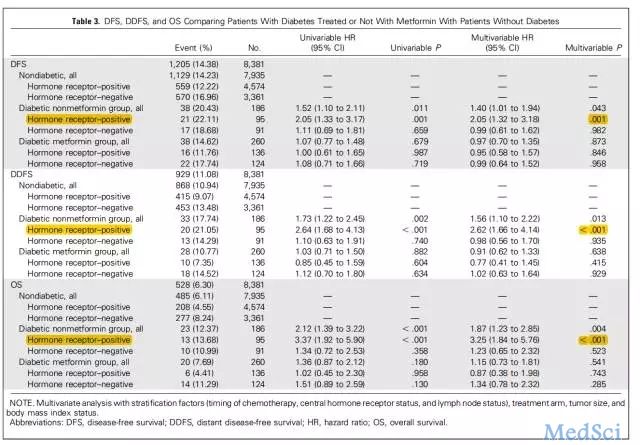
既往研究显示,糖尿病合并乳腺癌患者使用二甲双胍,可以改善患者生存结局。 近日,JCO杂志在线发文,纳入国际多中心大样本III期辅助治疗随机对照研究ALTTO的病例,探索性分析HER2阳性合并糖尿病的早期乳腺癌患者,二甲双胍治疗是否影响患者的复发和死亡风险。结果显示,在HER2阳性HR阳性合并糖尿病的早期乳腺癌患者中,服用二甲双胍治疗,对比未服药患者,复发和死亡风险更低。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCO#
40
感谢分享,学习了
75
#HER2阳性#
0
#糖尿病患者#
39
谢谢分享,学习了
75
非常好的研究
77
认真学习,谢谢分享
83