结合典型病例谈谈困难贲门失弛缓症内镜治疗进展
2019-09-24 青海涛 南方医院消化科青海涛大夫
目前,贲门失弛缓症比较主流的治疗方式是经口内镜下肌切开术,也就是POEM治疗,治疗效果较好,有效率达90%左右。因为POEM手术没有皮肤切口,仅通过内镜下贲门环形肌切开,可最大限度恢复食管生理功能,并减少手术并发症。术后早期就可进食,所以绝大部分患者术后吞咽困难可得到很好缓解,且反流性食管炎发生率比较低(约10%),创伤小、疗效可靠,是目前治疗贲门失弛缓症的最佳选择。如对中重度或者传统内镜下治疗效
前言
目前,贲门失弛缓症比较主流的治疗方式是经口内镜下肌切开术,也就是POEM治疗,治疗效果较好,有效率达90%左右。因为POEM手术没有皮肤切口,仅通过内镜下贲门环形肌切开,可最大限度恢复食管生理功能,并减少手术并发症。术后早期就可进食,所以绝大部分患者术后吞咽困难可得到很好缓解,且反流性食管炎发生率比较低(约10%),创伤小、疗效可靠,是目前治疗贲门失弛缓症的最佳选择。如对中重度或者传统内镜下治疗效果不佳的病人,可行外科Heller手术治疗,也就是贲门肌层切开术。
目前能熟练开展POEM的单位仍主要集中在少数大医院,其余医院仍处于经验积累阶段。已经已有一些文献针对以上困难报道,本文做了相应的总结并分享一些典型病例。
贲门失弛缓的概况
贲门失弛缓症的年发病率为每10万人1例,每10万人患病率为10例,这使其成为一种比较罕见的疾病。贲门失弛缓症患者的症状是由于下食管括约肌(LES)水平的流出道梗阻产生的。由于神经破坏,LES不会被正常的吞咽诱导而松弛,并且食管失去正常的蠕动功能。因此,食管排空只能基于重力来驱动。贲门失弛缓症的症状包括吞咽困难(固体和液体食物)、胸痛、体重减轻、烧心等,个别患者可并发吸入性肺炎及反流性咽炎。贲门失弛缓症可以是儿童或老人,年龄呈双峰分布,大多数患者在20~40岁和60~70岁,没有地域、种族和性别差异。
贲门失弛缓的治疗手段
贲门失弛缓症的各种治疗选择旨在通过降低LES中的静息压力来缓解症状。常规治疗包括口服药物治疗、硝酸盐和钙通道阻滞剂、肉毒杆菌毒素注射、球囊扩张术和外科Heller肌切开术。但口服药物、内镜下注射药物、球囊扩张和支架治疗等方法不能最终解除食管下端括约肌梗阻,疗效不肯定,复发率较高;外科手术切开食管下端括约肌疗效确切,但手术创伤大,恢复慢,住院时间长,手术费用也较高。经口内镜下食管括约肌切开术(per oral endoscopicmyotomy,POEM)为日本学者Inoue等人于2010年首先报道,因其不需要开胸、侵袭性低于外科Heller肌切开术,并且在体表不留疤痕等优点得以迅速普及。有限随访的初步研究报告认为95%~100%患者疗效满意,Eckardt症状评分显著改善,LES静息压降低。现在可以获得中期结果并确认POEM对症状的总体改善效果满意,但其疗效也随时间推移而降低。患者无需开胸手术,全部治疗过程均在插管麻醉状态下通过胃镜进行操作,手术时间短、创伤小。POEM微创手术的开展,不仅大大克服了传统治疗的疗效不确定性,而且恢复快、疗效可靠,充分体现了微创治疗的优越性。
困难病例的处理的研究进展
POEM手术的关键是成功建立足够长的黏膜下隧道而又不造成表面黏膜破损,隧道长度必须足以为肌切开术提供空间;肌切开术的长度至少为8~10厘米,在胃-食管交界处(GEJ)下方2~3厘米,以确保临床疗效。对于贲门失弛缓终末期合并乙状结肠型食管患者,由于食管腔明显扩张和扭曲,建立黏膜下隧道是困难的并且通常伴随有高概率的不良事件。首先,在弯曲部位难以建立黏膜下隧道;其次,扩张和弯曲的食管腔可能导致偏离方向,并且随后的内镜剥离和组织表面的分离是困难的;此外,先前接受过治疗的患者显示黏膜下层的炎症和纤维化可导致黏膜下隧道建立失败。
针对以上提出的难题,Kim等提出“两阶段POEM”法来应对,在较大弯曲区域的上部建立黏膜下隧道,然后在该区域进行肌切开术。随后,建立第二个黏膜下隧道,并在弯曲的下部再次进行肌切开术。最后,使钛夹进行创面封闭。
令狐恩强等提出通过短隧道法应对这种困难病例。短隧道的长度约为6-8厘米(上方4~6厘米,GEJ下方1~2厘米)。该研究纳入了126例LingIIc和III型贲门失弛缓症患者进行了回顾性研究。这些患者分为短隧道组(n=63)和标准隧道组(n=63)。短隧道组隧道和肌切开术的平均长度分别为7.6厘米和4.8厘米,标准隧道组分别为11.8厘米和9.2厘米。短隧道组的平均手术时间明显短于标准隧道组(39.5min vs. 48.2min,P=0.001)。两组间手术相关不良事件发生率有显著差异(9.5% vs. 33.3%,P=0.001)。POEM后,两组之间的Eckardt评分,LES基础压力或残余压力的变化无显著差异,短隧道手术时间短和手术相关不良事件的发生率明显减少。
对于严重黏膜下纤维化无法建立隧道的患者,胡兵等探索了一种没有黏膜下隧道的方法,将其称为开放式经口内镜下肌切开术(O-POEM)。纳入了82例行O-POEM患者进行了分析。治疗成功定义为肌切开术后Eckardt评分小于或等于3。中位随访18个月(范围:6~26个月)后,治疗成功率(Eckhart评分≤3)达到96.3%,治疗前后平均评分(7.4 vs. 1.8 ; P<0.001),复发3例。10名患者(12.2%)患有不良事件,其中2例为纵隔炎,1例为O-POEM出血,1例皮下气肿,6例胸腔积液。两例纵隔炎需要引流,其他患者通过内镜检查和保守治疗,没有死亡和中转手术的病例,15.9%的患者发生临床反流(13/82)。该研究提示O-POEM治疗贲门失弛缓症是可靠和有效的,尤其是对于无法建立隧道的困难病例可能更加适用。
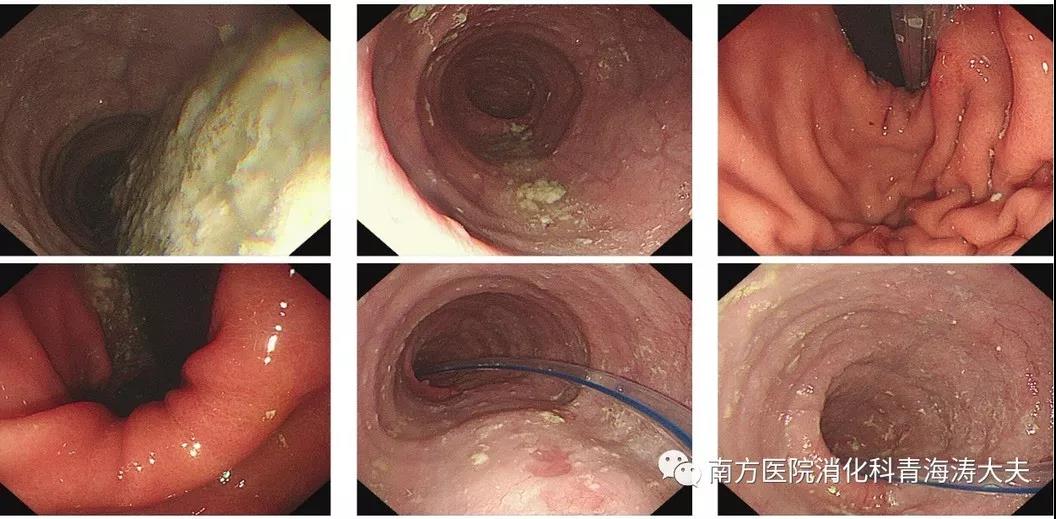
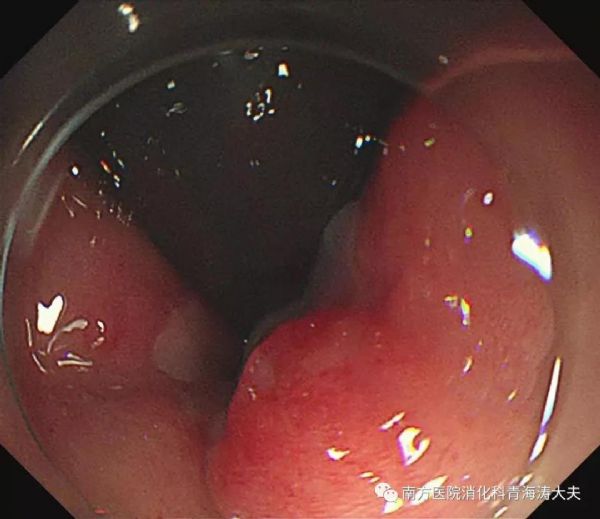
普通贲门失弛缓症病例POEM手术过程。
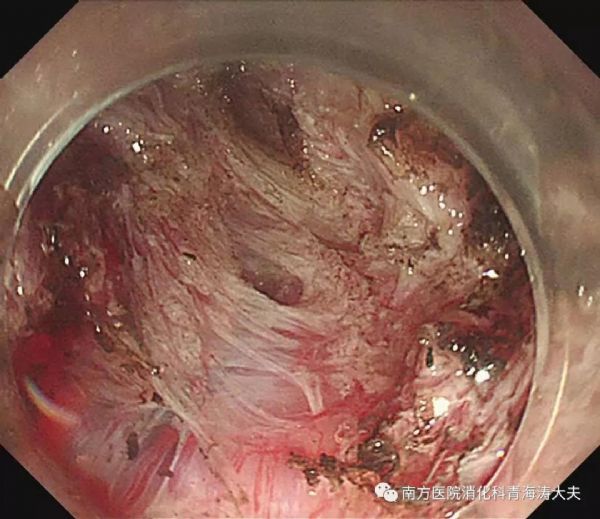
术前患者食管管腔内存在大量食物
POEM手术过程,手术耗时约30min
典型困难病例分享
病例1 黏连病例
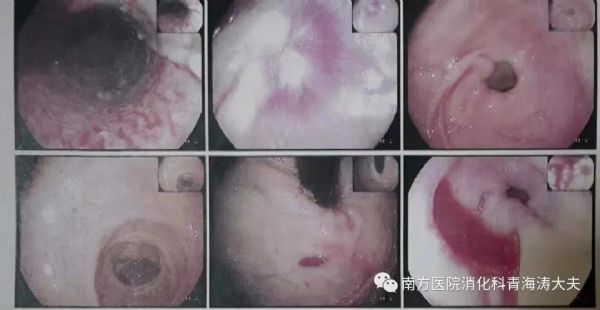
患者李某,男性,60岁,罹患贲门失弛缓症数年。既往食管撕裂史,扩张史,食管中下段疤痕明显。以下是既往胃镜报告。
术前原本预计open-POEM术,如有其他情况则转外科行heller术,克服贲门附近约4cm长黏连带,先切开肌层,再小心分离与黏膜下层黏连的部分环形肌后顺利到达胃底3cm处,最终顺利完成手术。手术耗时约1小时。术后数月余,随访效果良好!
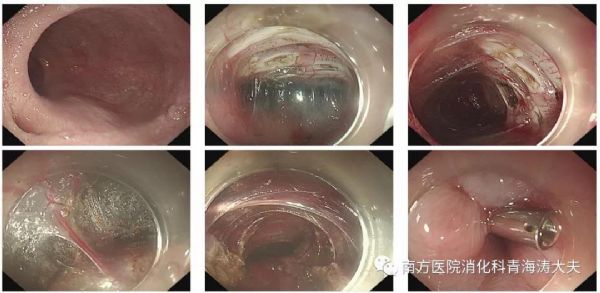
手术过程如下:
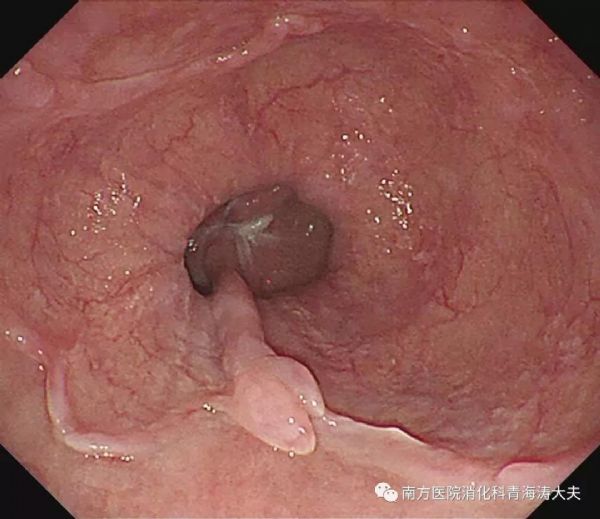
病例2 外科heller肌切开术后黏连病例
患者赵某,女性,40岁,罹患贲门失弛缓症数年,去年当地外科heller肌切开术后效果欠佳,POEM手术过程中隧道中上段黏连较明显(下图上部中间图片),小心切开至隧道下段又豁然开朗!手术耗时约35分钟!手术过程如下:
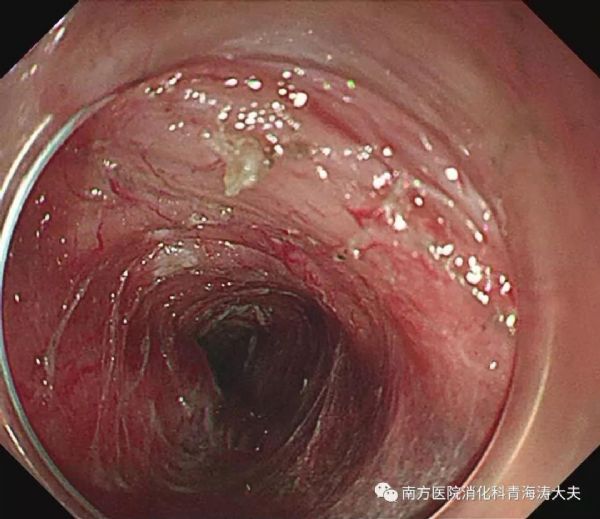
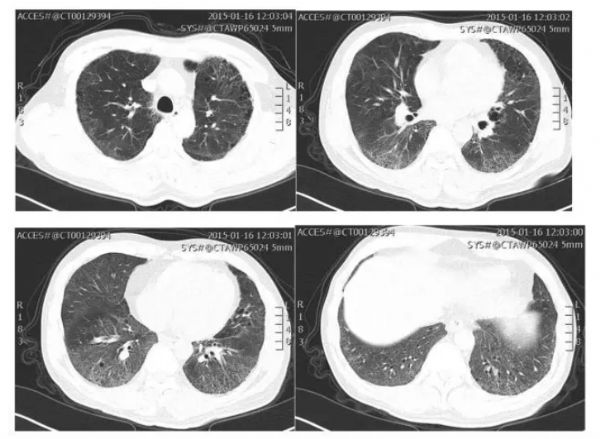
病例3 乙状结肠型病例
患者谢某,男性,38岁,罹患贲门失弛缓症数年。术中可见食管腔明显扩张、扭曲,呈乙状结肠型,内镜可见食管腔内倒镜,手术耗时1小时余。手术过程如下:
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
0
#贲门#
31
#内镜#
35
#内镜治疗#
49
#贲门失弛缓症#
37