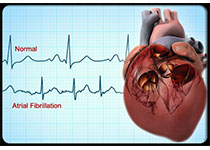
BMJ:房颤患者服用口服直接抗凝药对中风的预防效果研究
2017-11-29 zhangfan MedSci原创
研究人员对房颤患者接受口服直接抗凝药(DOACs)对中风的预防效果进行了系统综述和荟萃分析,大多数DOAC的效果优于华法林,其中5mg每天2次的阿哌沙班最具成本效益
近日研究人员考察了房颤患者服用口服直接抗凝药(DOACs)对中风的预防效果。本次研究为系统综述和荟萃分析,房颤患者服用DOACs、维生素K拮抗剂或抗血小板药物对中风预防效果的临床研究入选。23项临床研究,总计94656名患者参与本次研究,其中13项研究比较了DOACs与华法林在达到目标INR2.0-3.0时的剂量。研究发现,5mg每天2次的阿哌沙班(OR 0.79, 95% CI 0.66-0.94), 150mg每天2次的达比加群 (0.65, 0.52-0.81), 60mg每天1次的依度沙班 (0.86, 0.74-1.01)以及20mg每天1次的利伐沙班(0.88, 0.74-1.03),与华法林相比,可降低中风或全身栓塞的风险。相比于150mg每天2次的达比加群,患者服用60mg每天1次的依度沙班(1.33, 1.02-1.75)以及20mg每天1次的利伐沙班(1.35, 1.03-1.78)其中风或全身栓塞的风险增加。所有DOAC相比于华法林均可降低患者全因死亡风险,5mg每天2次的阿哌沙班(0.71,0.61-0.81), 110mg每天2次的达比加群 (0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BMJ#
31
#房颤患者#
31
学习了受益匪浅
70
学习啦!谢谢分享!
67
学习一下谢谢分享
74
学习.
61
学习了.谢谢分享.
72