心血管疾病(CVD)是全球致死第一大原因。虽然随着医学的发展,高收入国家CVD疾病负担在下降,但中低收入国家(LMICs)的疾病负担却在上升。数据显示,2017年因CVD的死亡人数为1780万,年龄标准化死亡率为233/10万。
与高收入国家相比,LMICs的CVD患者更年轻,且在疾病负担和管理经济困难方面都表现出明显的社会经济梯度。此外,世界卫生组织(WHO)提出“到2030年将非传染性疾病(NCDs)的过早死亡率降低三分之一”的目标。
由于CVD给患者家庭甚至全社会的经济负担都不断增加,因此了解CVD风险在全球范围内的差异,显得尤为重要。为此,来自澳大利亚新南威尔士大学、美国斯坦福大学及德国海德堡大学等机构的权威专家对45个LMICs的CVD风险和管理概况进行了全面分析与评估,结果发表在最新的发表在美国科学公共图书馆杂志PLOS Medicine杂志上。
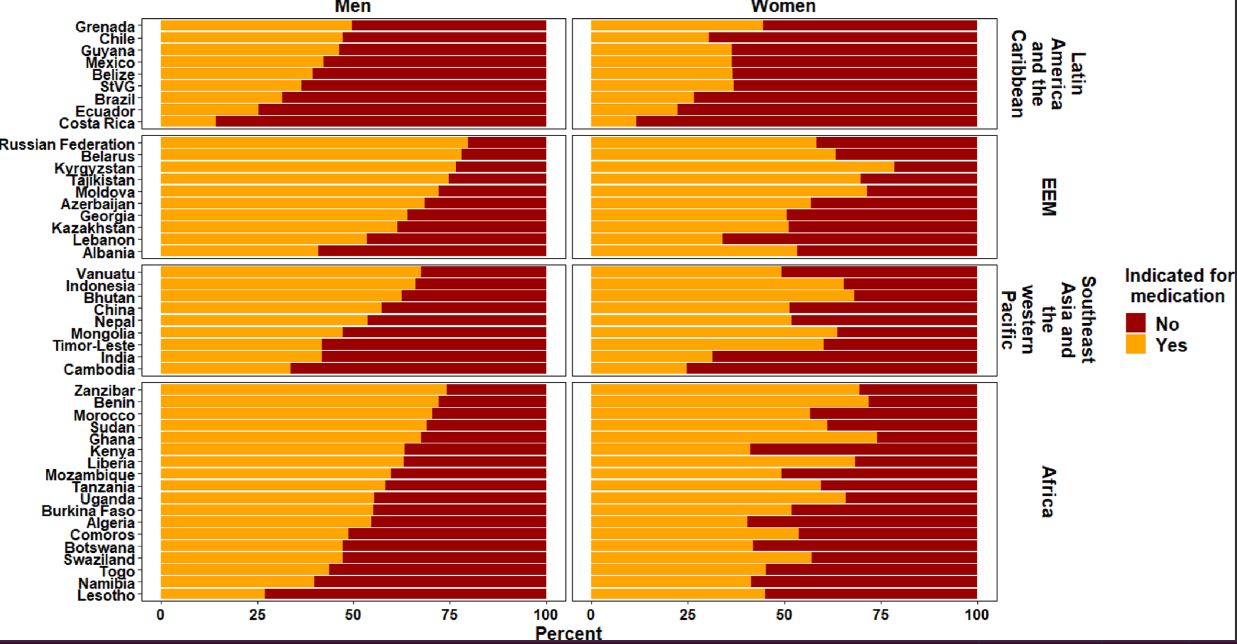
研究人员对2005年至2017年期间开展的45个LMICs具有全国代表性的家庭调查进行了横断面分析,其中32项调查为WHO下属逐步监测法(STEPS)研究。根据2019年WHO CVD风险图工作组方程计算出国别10年CVD风险中位数,高血压用药指征基于WHO基本非传染性疾病干预指南评估。
共分析了包括来自45个国家的600484名成人完整病例。总的来说,CVD风险状况差异很大。男性和女性10年CVD风险中位数分别为2.7%(2.3%-4.2%)和1.6%(1.3%-2.1%),其中撒哈拉以南非洲地区风险最低,而欧洲和东地中海地区风险最高。
在大多数国家,教育程度和就业率与CVD风险呈负相关。即教育程度高和高就业率往往CVD风险降低。在45个研究国家中,大多数国家的降压药物使用与社会人口特征之间没有关联。
最让人意外的是,在所有国家,CVD风险高的人往往用药不足(只有24.2%和41.6%的男女性高CVD风险患者服用指南推荐的降压药),而CVD风险较低的人则用药过度,47%的CVD较低风险的人过度服用不符合指南要求的降压药。
综上,该研究提示,LMICs需要针对具体国情制定有针对性的政策,以帮助识别并改善心血管疾病情况。
参考文献:
Peiris D, et al. Cardiovascular disease risk profile and management practices in 45 low-income and middle-income countries: A cross-sectional study of nationally representative individual-level survey data. PLoS Med. 2021 Mar 4;18(3):e1003485. doi: 10.1371/journal.pmed.1003485.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血管病#
27
#药物使用#
26
#降压#
16
#Med#
20