NEJM:丙肝药物Sofosbuvir和Velpatasvir联用大获成功,肝硬化依然有效(ASTRAL系列研究)
2015-12-02 MedSci MedSci原创
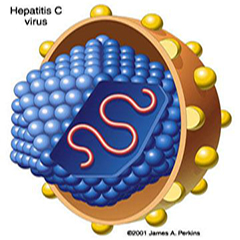
人们首次认识到丙肝这种疾病是在上世纪七十年代,这是一种经血液传播的非甲非乙型肝炎病毒,是引起输血后肝炎的主要病因之一。1989年,人们首次鉴定到了丙肝病毒(HCV)。这种病毒善于躲避患者机体的免疫系统,能够建立长达数十年的感染。这种持续性的感染会损伤肝脏,甚至引发肝癌。绝大多数感染者起初并不表现出症状,直到病毒引起严重的肝脏损伤。贝斯以色列女执事医疗中心(BIDMC)和Intermountain医
人们首次认识到丙肝这种疾病是在上世纪七十年代,这是一种经血液传播的非甲非乙型肝炎病毒,是引起输血后肝炎的主要病因之一。1989年,人们首次鉴定到了丙肝病毒(HCV)。这种病毒善于躲避患者机体的免疫系统,能够建立长达数十年的感染。这种持续性的感染会损伤肝脏,甚至引发肝癌。绝大多数感染者起初并不表现出症状,直到病毒引起严重的肝脏损伤。
贝斯以色列女执事医疗中心(BIDMC)和Intermountain医学中心的研究人员最近发现,使用特定的抗病毒药物组合,能够在超过90%的晚期肝病患者中根除丙肝感染。这项名为ASTRAL系列的临床研究(ASTRAL-1,-2,-3,-4)以3篇研究论文形式同时发表在同一期《新英格兰医学》(NEJM)上。不仅证明对不同基因型丙肝有很好疗效,就连进展到肝硬化的患者而言,依然疗效很好。此前报道:NEJM:Sofosbuvir和Velpatasvir治疗HCV感染有较高的病毒学应答率 和 HCV基因型2或3患者——sofosbuvir/velpatasvir优于标准治疗方案
全世界有上亿人受到丙肝病毒的感染,这种感染会引起肝功能衰竭和肝硬化。当患者的健康肝脏组织被瘢痕组织取代,肝功能衰竭和肝硬化就会发生,最终使肝脏无法正常执行自己的功能。
据介绍,总共有267名肝功能衰竭的患者参与了这项临床研究。“对于已经出现肝硬化和肝功能衰竭的丙肝患者来说,可选择的治疗方式其实很少,”Curry说。“在我们这项研究中,大部分参与者的肝功能都出现了改善。这种改善体现在Child-Pugh评分和MELD评分上,Child-Pugh评分主要评估肝硬化的严重性,MELD评分用于确定患者在肝移植中的优先次序。”
肝脏是人体内最大的实体器官,起到了许多关键性的作用,包括生产血蛋白促进凝血和免疫系统功能、生成胆汁帮助机体消化食物、以及储存产能的葡萄糖。此外,肝脏还为机体排出酒精等有害物质。
“因为丙肝发生肝功能衰竭的患者,在未来十年将大大增加,”Curry说。“我们的研究表明,晚期肝病患者依然可以从丙肝治疗中获益,根除丙肝感染有助于肝功能的改善。”
这项研究也引起了我国传染病专家的广泛关注,有专家评论道:“最近丙型肝炎的抗病毒药物很多,开启了丙肝治疗的新纪元”。
原始出处:
Foster GR, Afdhal N, Roberts SK, Bräu N, Gane EJ, Pianko S, Lawitz E, Thompson A, Shiffman ML, Cooper C, Towner WJ, Conway B, Ruane P, Bourlière M, Asselah T, Berg T, Zeuzem S, Rosenberg W, Agarwal K, Stedman CA, Mo H, Dvory-Sobol H, Han L, Wang J, McNally J, Osinusi A, Brainard DM, McHutchison JG, Mazzotta F, Tran TT, Gordon SC, Patel K, Reau N, Mangia A, Sulkowski M; ASTRAL-2 and ASTRAL-3 Investigators.Sofosbuvir and Velpatasvir for HCV Genotype 2 and 3 Infection.N Engl J Med. 2015 Nov 17
Feld JJ, Jacobson IM, Hézode C, Asselah T, Ruane PJ, Gruener N, Abergel A, Mangia A, Lai CL, Chan HL, Mazzotta F, Moreno C, Yoshida E, Shafran SD, Towner WJ, Tran TT, McNally J, Osinusi A, Svarovskaia E, Zhu Y, Brainard DM, McHutchison JG, Agarwal K, Zeuzem S; ASTRAL-1 Investigators.Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection.N Engl J Med. 2015 Nov 16.
Curry MP, O'Leary JG, Bzowej N, Muir AJ, Korenblat KM, Fenkel JM, Reddy KR, Lawitz E, Flamm SL, Schiano T, Teperman L, Fontana R, Schiff E, Fried M, Doehle B, An D, McNally J, Osinusi A, Brainard DM, McHutchison JG, Brown RS Jr, Charlton M; ASTRAL-4 Investigators.Sofosbuvir and Velpatasvir for HCV in Patients with Decompensated Cirrhosis.N Engl J Med. 2015 Nov 16.
Pianko S, Flamm SL, Shiffman ML, Kumar S, Strasser SI, Dore GJ, McNally J, Brainard DM, Han L, Doehle B, Mogalian E, McHutchison JG, Rabinovitz M, Towner WJ, Gane EJ, Stedman CA, Reddy KR, Roberts SK.Sofosbuvir Plus Velpatasvir Combination Therapy for Treatment-Experienced Patients With Genotype 1 or 3 Hepatitis C Virus Infection: A Randomized Trial.Ann Intern Med. 2015 Dec 1;163(11):809-17.
Pianko S, Flamm SL, Shiffman ML, Kumar S, Strasser SI, Dore GJ, McNally J, Brainard DM, Han L, Doehle B, Mogalian E, McHutchison JG, Rabinovitz M, Towner WJ, Gane EJ, Stedman CA, Reddy KR, Roberts SK.Sofosbuvir Plus Velpatasvir Combination Therapy for Treatment-Experienced Patients With Genotype 1 or 3 Hepatitis C Virus Infection: A Randomized Trial.Ann Intern Med. 2015 Dec 1;163(11):809-17.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
33
#AST#
31
#Velpatasvir#
24
#丙肝药#
40
是一篇不错的文章
109
值得进一步关注
80
这篇文章有一定深度
117
不错,赞一个
100
赞一个
95
好文章,值得收藏
79