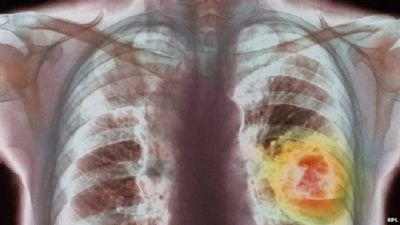
BBC:肺癌治疗的里程碑新发现
2015-06-01 孟小猫 译 医学论坛网
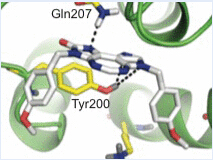
2015年5月30日,据BBC新闻报道的一项新近研究称,肺癌治疗可使一些患者的生存期加倍,实属里程碑式的新发现。 Nivolumab可使隐藏与人体正常防御系统之下的癌细胞无所遁形,让其接受人体免疫系统的自发处理。 该结果来自纳入582例癌症患者的研究结论,在美国临床肿瘤学
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#里程碑#
24
#肺癌治疗#
24
#新发现#
27
确实里程碑的进展
89
恩恩
47
没讲清楚
159
期待
160