ACC:首次证实!阿司匹林可降低糖尿病和心衰患者死亡风险,但……
2018-03-03 Chen 生物探索
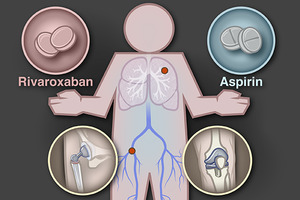
发表在美国心脏病学会第67届年度科学会议上的一项研究称,对患有2型糖尿病和心力衰竭的人来说,每天服用阿司匹林似乎能够降低死亡或因心衰住院的风险。但数据也显示,阿司匹林的使用可能会增加患非致命性心脏病或中风的风险。这一有点矛盾的发现,让研究人员感到惊讶。
作为医药史上三大经典药物之一,阿司匹林起初以镇痛消炎为主要功效,逐渐又被发现有抗血栓的作用。现在,阿司匹林被强烈推荐给那些先前患有心脏病或中风的患者,但对于那些有心血管风险因素但并没有心脏病发作或中风病史的患者来说,阿司匹林的使用指南还不清楚。
在美国,有约2700万2型糖尿病患者,且约有650万美国成年人患有心力衰竭。这两种疾病都与心脏事件(包括心脏病发作和中风)升高的风险有关。这项评估“阿司匹林作为糖尿病和心力衰竭患者一种预防措施”的首个研究,揭示了阿司匹林对这两类患者的潜在风险和益处。
具体来说,利用来自The Health Improvement Network的数据,研究人员提取了12,000多名年龄≥55岁的2型糖尿病和心力衰竭患者(这些患者先前无心脏病、中风、外周动脉疾病或房颤病史)的健康记录。其中,大约一半的人每天服用阿司匹林,一半人没有。经过平均5年的随访,研究人员分析了他们的健康结果。
结果显示,每天服用阿司匹林的患者,其全因死亡率和因心力衰竭的住院率(All-cause mortality and hospitalization for heart failure)降低了10%,但非致命性心脏病发作或中风发作却增加了50%。
领导该研究的Charbel Abi Khalil博士说:“服用阿司匹林导致死亡率下降的同时,也带来了非致命性心脏病发作和中风发作矛盾的增长。这让我们非常惊讶。这可能是因为,对于寿命更长的患者(平均年龄为70岁),他们倾向于发生更多的心脏事件。”
不过,这项研究也有局限性,因为它是基于对健康记录的回顾性分析,而不是基于一项随机对照试验。进一步的研究将有助于证实这一发现,并可能为糖尿病和心力衰竭患者的治疗提供具体的指导方针。但就目前来说,Abi Khalil认为,患者应该于他们的医生进行交流,以评估服用阿司匹林的益处和风险。
原始出处:
Aspirin lowers risk of death for patients with diabetes, heart failure.American College of Cardiology.Feb 28, 2018
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#首次证实#
43
#患者死亡#
41
#死亡风险#
38
#ACC#
43
#心衰患者#
37
指南早就指出了这一点
65