European Radiology:使用机器学习,预测Stanford B型主动脉夹层TEVAR术后的再干预风险
2022-02-14 shaosai MedSci原创
主动脉夹层是一种高度致命性疾病,每年的发病率为每10万人中有2至6人。目前,胸腔内主动脉修复术(TEVAR)是复杂的斯坦福B型主动脉夹层(TBAD)患者的首选疗法。
 主动脉夹层是一种高度致命性疾病,每年的发病率为每10万人中有2至6人。目前,胸腔内主动脉修复术(TEVAR)是复杂的斯坦福B型主动脉夹层(TBAD)患者的首选疗法。然而,TEVAR后的术后并发症发生率很高。再次介入的发生与术后并发症密切相关,并增加了主动脉破裂的风险。
主动脉夹层是一种高度致命性疾病,每年的发病率为每10万人中有2至6人。目前,胸腔内主动脉修复术(TEVAR)是复杂的斯坦福B型主动脉夹层(TBAD)患者的首选疗法。然而,TEVAR后的术后并发症发生率很高。再次介入的发生与术后并发症密切相关,并增加了主动脉破裂的风险。
目前,虽然没有制定再介入的标准诊断和治疗指南,但对于TEVAR术后出现严重并发症的患者,进行再介入治疗已成为共识。术前CTA和术后即刻主动脉数字减影血管成像(DSA)的特点对于TEVAR后TBAD患者的治疗策略和随访具有重要意义。
然而,很少有研究将TEVAR前的CTA与TEVAR后的即刻DAS结果结合起来,以分流或预测患者进行再介入的风险。大量的数据需要机器学习来改善和加速心血管疾病的诊断、治疗和预后。这种方法提供了一套强大的工具来解开变量和结果之间的关系,使预测更加准确。
近日,发表在European Radiology杂志的一项研究根据临床、术前CTA和术后DSA的特征,开发并验证了预测TBAD的TEVAR术后再次介入的分类模型,为临床医生成功预测再干预的风险、并进一步优化高风险患者的监测和治疗提供了可能。
本研究共纳入192名接受TEVAR手术的TBAD患者;68人(35.4%)有接受再介入的指征。收集了临床特征、术前和术后CTA的主动脉特征,以及术后立即进行的DSA特征。应用最小绝对收缩和选择算子(LASSO)回归法来确定再次干预的风险因素。八个分类器被用于建模。这些模型在100个训练-验证的随机分片上训练,比例为2:1。通过受试者工作特征曲线来评估其性能。
确定了七个再干预的预测因素,包括最大假腔直径、在左锁骨下动脉远端约15毫米处测量的主动脉直径、在膈肌水平测量的主动脉直径、在腹腔动脉水平测量的假腔直径、裸金属和覆盖支架的数量、裸金属支架的数量以及假腔的残余灌注。Logistic回归(LR)的性能最高,曲线下面积为0.802。一个为临床使用而建立的列线图显示出良好的校准。将患者分为低风险和高风险亚组的分界值为0.413。Kaplan-Meier曲线显示,高危患者的总生存期明显短于低危患者(均为P < 0.05)。
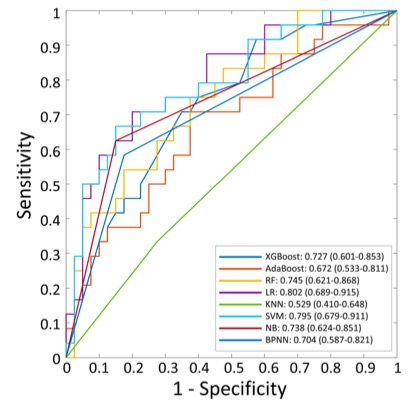
图 验证队列中分类器的受试者工作特征曲线。
本项研究表明,在选择TBAD患者进行TEVAR和制定术后监测策略时,应综合考虑临床特征、CTA的特征和术后即刻DSA的特征。本研究开发并验证了一个用于预测TBAD患者在TEVAR术后再介入概率的列线图。该列线图可将患者分为低风险或高风险亚组,其中高风险患者的OS明显高于低风险患者。
原文出处:
Yuhao Dong,Lifeng Que,Qianjun Jia,et al.Predicting reintervention after thoracic endovascular aortic repair of Stanford type B aortic dissection using machine learning.DOI:10.1007/s00330-021-07849-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
22
#B型主动脉夹层#
31
#Stanford#
39
楼主你好,可以分享一下原文吗?谢谢
33
#TEVAR#
27
#主动脉#
0
#动脉夹层#
43
#机器#
27