UICC/AJCC 2017年第八版食管癌 TNM 分期标准
2017-07-05 MedSci MedSci原创
1987 年开始,国际抗癌联盟(Union for International Cancer Control,UICC)与美国癌症联合会(American Joint Committee on Cancer,AJCC)联合发布恶性肿瘤 TNM 分期标准,并不定期更新。目前,临床上采用的最新版食管癌 TNM 分期标准是 2009 年第 7 版。近日食管癌第 8 版 TNM 分期的初稿近期布在 J
1987 年开始,国际抗癌联盟(Union for International Cancer Control,UICC)与美国癌症联合会(American Joint Committee on Cancer,AJCC)联合发布恶性肿瘤 TNM 分期标准,并不定期更新。目前,临床上采用的最新版食管癌 TNM 分期标准是 2009 年第 7 版。近日食管癌第 8 版 TNM 分期的初稿近期布在 Journal of Thoracic Oncology 杂志上。详细中文指南下载:2017年UICC/AJCC 第8版肺癌/食管癌TNM分期标准
食管上皮及食管胃结合部上皮源性肿瘤第 8 版分期分别对临床、病理及新辅助治疗后进行分期,不再使用共同的分期系统。
对于病理 TNM 分期,pT1 分为 pT1a 及 pT1b 以便对 I 期腺癌及鳞癌进行亚组分析。并介绍全新的区域淋巴结图谱。弃用组织学表现为未分化型(G4)这一术语;组织病理细胞学类型需要更深层的分析。
分期为 pT2N0M0 的鳞癌,肿瘤位置将不作为分期指标。食管胃交界的定义将会进行修订。ypTNM 分期系统不区分不同组织学类型,腺癌及鳞癌共用一个分期系统。
肿瘤分类
表 1-6 对分类的标准做了定义。解剖学上的食管癌分类项目包括原发性肿瘤(T),区域淋巴节(N)和远处转移(M)(图1)。 pT1 重新定义,细分为 pT1a 和 pT1b。
图 1 第八版 TNM 分类。
注:T 分期分为 Tis:高度不典型增生;T1:癌症侵犯黏膜固有层,粘膜肌层或粘膜下层,并被分为 T1a(癌症侵犯黏膜固有层或粘膜肌层)和 T1b(癌侵犯粘膜下层);T2:癌侵犯固有肌层;T3:癌症侵犯外膜;T4:癌侵入局部结构并且被分类为 T4a:癌侵入相邻结构例如胸膜,心包膜,奇静脉,膈肌或腹膜,T4b:癌侵入主要相邻结构,例如主动脉,椎体或气管。
N 分类为 N0:无区域淋巴结转移; N1:涉及 1?2 个区域淋巴结转移; N2:涉及 3-6 个区域淋巴结转移;N3:涉及 7 个或以上区域淋巴结转移。
M 分类为 M0:无远处转移;M1:远处转移
表 1 原发肿瘤(T)分期
表 2 区域淋巴结(N)分期
表 3 远处转移(M)分期
表 4 食管鳞癌位置分类 ,位置定义以肿瘤中心为参考
表 5 食管腺癌分化程度,*如果对“ 未分化”癌组织的进一步检测为腺体组织,则分类为 G3 腺癌
表 6 食管鳞癌分化程度,*如果对“ 未分化”癌组织进一步检测为鳞状细胞组分,或如果在进一步检测后仍为未分化癌,则分类为 G3 鳞癌
新的淋巴图谱阐述位于上食管括约肌至腹主动脉间的食管外膜(食管周围组织)周围的淋巴结(图2)。7 版的淋巴图谱存在问题,因其涵盖了不属于食管区域淋巴结的肺淋巴结。
图 2 食管癌淋巴结图谱 食管癌分期区域淋巴结站点:左面观(A),右面观(B)及前面观(C)。
注:1R:右侧下颈段气管旁淋巴结,位于锁骨气管旁与肺尖之间;1L 对于左侧相同位置;2L:左上气管旁淋巴结,位于主动脉顶点与肺尖之间;4R:右下气管旁淋巴结,位于头臂动脉的尾部边缘气管交叉点与奇静脉的头部边缘之间;4L:左下气管旁淋巴结,位于主动脉顶点与隆突之间;
7:隆突下淋巴结,气管隆突下方;8U:上胸段食管旁淋巴结,自肺尖至气管分杈;8M:中胸段食管旁淋巴结,自气管分杈处至下肺静脉边缘;8Lo:下胸段食管旁淋巴结,位于自下肺静脉尾部边缘至食管胃交界区;
9R:右下肺韧带淋巴结,在右下肺韧带内;9L:左下肺韧带淋巴结,在左下肺韧带淋巴结内;15:膈肌淋巴结,位于膈穹隆及膈脚后面或连接处;16:贲门旁淋巴结,紧邻胃食管交界区;17:胃左淋巴结,延胃左动脉走行分布;18:肝总动脉淋巴结,位于近端肝总动脉。
19:脾淋巴结位于近端脾动脉;20:腹腔淋巴结,位于腹主动脉旁;颈段食管旁 5,6 级淋巴结根据头颈部淋巴结命名法命名
早期食管癌的病理分期(pTNM),肿瘤分级(G 分期)尤为重要。未分化癌对组织病理学细胞类型需要更多的分析。 如果可以确定起源于何种腺体,该癌症被分期为 3 级腺癌;如果可以确定为鳞状起源或最终仍评估为未分化癌,则分为 3 级鳞状细胞癌。
肿瘤位置对于腺癌分期作用不大。但是肿瘤位置联合 G 分期对 pT1-3N0M0 鳞癌再分期必不可少。食管胃交界区被重新定义,肿瘤中心距离胃贲门 ≤ 2 cm 按照食管腺癌进行分期;超过 2 cm 应按照胃癌进行分期(图 3)。
图 3 食管癌原发灶位置,通常使用肿瘤到门齿的距离表示。精确的测量取决于身材大小和身高。 肿瘤原发部位的位置由癌症中心定义。 涉及食管胃交界(EGJ)的癌症,其中心在贲门的近端 2 cm 内(Siewert 类型 I / II)将被分期为食管癌。 正中距离 EGJ 远于 2 cm 的癌症,即使涉及 EGJ,也将使用胃癌的 TNM 分期进行分期
分期
病理分期组(pTNM)
过去食管切除术后病理分期是肿瘤分期的唯一标准。今天,病理分期正在失去其临床相关性,因为在晚期肿瘤患者,辅助治疗取代了单纯食管切除术。然而,它仍然与早期癌症的分期与预后息息相关。
腺癌:
亚分期中 8 版分期比 7 版分期多 1 种(图 4A)。病理 0 分期限定为高度不典型增生(pTis)。
T1 亚型结合 G 分期将Ⅰ期分 3 个亚组:IA 期(pT1aN0M0 G1),IB 期(pT1aN0M0 G2 及 pT1bN0M0 G1-2),IC 期(pT1N0M0 G3 和 pT2N0M0 G1-2)。pT2N0M0 G3 仍为ⅡA 期的唯一亚型。
T3N0M0 和 pT1N1M0 构成 IIB 期。III 期因预后相对较好予以保留。IIIA 期包括 pT2N1M0 和 pT1N2M0,而 pT2N2M0,pT3N1-2M0 和 pT4aN0-1M0 构成 IIIB 期。
因大多数的局部晚期病例与远处转移(M1)的有相似生存期,同属 IV 期。pT4aN2M0,pT4bN0-2M0 和 pTanyN3M0 为 IVA 期。远处转移(M1)为 pStage IVB。
图 4A 腺癌病理 TNM 分期
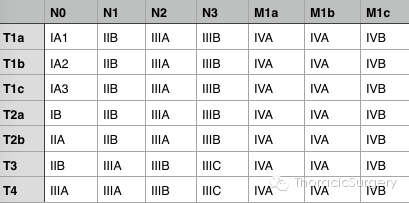
鳞癌:
第 8 版分期亚型数量无增减,但进行重排和重命名(图 4B)。0 期仅限于高度不典型增生即 pTis。T1 期结合 G 分期将 I 期分为 2 组:IA 期(pT1aN0M0 G1)和 IB 期(pT1aN0M0 G2-3,pT1bN0M0 和 pT2N0M0 G1)。
下胸段 pT2N0M0 G2-3,pT3N0M0 和中上胸段 pT3N0M0 G1 食管癌组成 IIA 期。IIB 期包括上胸段食管的 T3N0M0 G2-3 及 pT1N1M0。III 期和 IV 期分类方法同腺癌。
图 4B 鳞癌病理 TNM 分期
新辅助病理分期(ypTNM)
8 版分期创新之处在于对接受新辅助治疗且有病理活检的病例进行单独分期(图 5)。这种添加驱动因素包括特异性新辅助后的病理类别(ypT0N0-3M0 和 ypTisN0-3M0),不同阶段组成分和显着不同的生存概况等同于病理(pTNM)类别的缺失。
此分组不考虑组织病理学细胞类型。G 分期不包括在新辅助后病理分期中。 yp I 期包含 ypT0-2N0M0。ypII 期即 ypT3N0M0。
yp IIIA 期包括限于食管壁,具有 ypN1 区域淋巴结(ypT0-2N1M1)的食管癌。ypIIIB 期包含 ypT1-3N2M0,ypT3N1M0 和 ypT4aN0M0。ypIVA 期包括 ypT4aN1-2M0,ypT4bN0-2M0 和 yp TanyN3M0。ypIVB 期包含 ypM1。
图 5 腺癌及鳞癌新辅助病理 TNM(ypTNM)分期
临床分期(cTNM)
临床分期主要用于肿瘤组织学数据缺失的情况下,TNM 分类通常基于影像学资料而非病理学资料。临床分期(cTNM)与病理分期(pTNM)存在不同分期和生存期资料。
腺癌:
临床分期 0 期包含 cTis(图 6A)。 临床分期 I 期即 cT1N0M0。临床分期 IIA 期为 cT1N1M0,临床分期 IIB 期为 cT2N0M0。
临床分期 III 期包括 cT2N1M0 和 cT3-4aN0-1M0。 T4bN0-1M0 和所有 cN2-N3M0 属于临床分期 IVA 期。临床分期 IVB 期包含所有 cM1。
图 6A 腺癌临床 TNM 分期
鳞癌:
临床分期 0 期包含 cTis(图 6B)。 临床分期 I 期即 cT1N0-1M0。 临床分期 II 期包含 cT2N0-1M0 和 cT3N0M0。
临床分期 III 期包含 cT3N1M0 和 cT1-3N2M0。 cT4N0-2M0 和所有 cN3M0 属于临床分期 IVA 期。临床分期 IVB 期包含所有 cM1。
图 6B 鳞癌临床 TNM 分期
结论
第 8 版食管癌和食管癌的分期有数据支持,对第 7 版病理分期(pTNM)进行扩展,同时包括新辅助治疗(ypTNM)病理分期及治疗前的临床分期(cTNM)(表 7)。
表 7 第八版与第七版的不同点
|
pTNM |
分类 |
T |
T1 分为 T1a 和 T1b, 进一步细分为 IA 和 IB 期鳞癌和 IA-IC 期腺癌。 |
|
删除 T2 期鳞癌肿瘤位置对分期的影响。 |
|||
|
T4a 期包括直接侵犯腹膜。 |
|||
|
G |
删除 G4 分期,并且需更多的检测确定腺状(G3 腺癌)或鳞状(G3 鳞癌)分化。 如果为未分化,则被归为 G3 鳞癌。 |
||
|
L |
食管胃交界处肿瘤中心距胃贲门近端 2 cm 内则按食管癌分期。食管胃交界处肿瘤中心距胃贲门>2 cm 即使侵犯食道,被归为胃癌,其在第 7 版中归为食管癌。 |
||
|
分期 |
Ⅲ |
删除第 7 版中的ⅢC 期 |
|
|
Ⅳ |
进一步细分为ⅣA 期及ⅣB 期 |
||
|
ypTNM |
分期 |
AⅡ |
与 pTNM 不同,腺癌及鳞癌分期相同 |
|
cTNM |
分期 |
AⅡ |
与 pTNM 不同,腺癌及鳞癌分期也不同 |
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


























#UICC#
35
学习了谢谢作者分享!
75
#TNM#
47
#AJCC#
45
#食管#
27
#ICC#
27
推广!
71
很实用的文章
86