颈动脉斑块需要他汀治疗吗?
2017-10-27 郭艺芳 郭艺芳心前沿
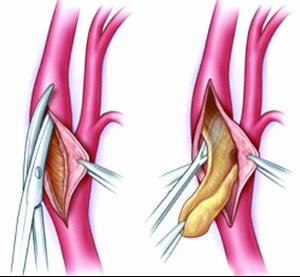
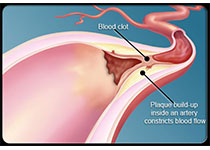
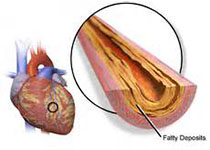
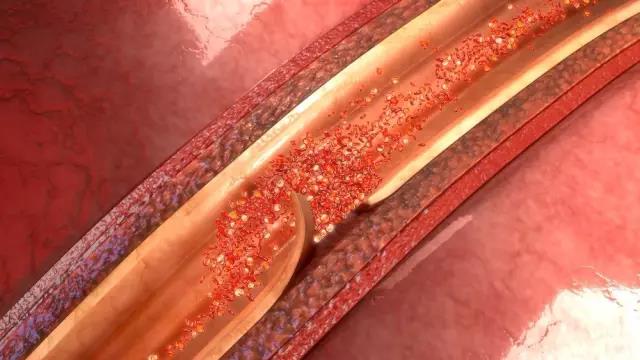
近年来颈动脉超声检查普遍开展,很多患者或健康查体者被发现有颈动脉斑块。存在颈动脉斑块者需要应用他汀治疗吗?这是临床上经常被患者问到的问题。这个问题无法一概而论,应结合患者的颈动脉狭窄程度、是否存在心血管病或心血管病危险因素以及低密度脂蛋白胆固醇(LDL-C)水平综合考虑。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









感谢分享
61
#颈动脉#
31
#颈动脉斑块#
36
#斑块#
33
学习了新知识学习了新知识
49
谢谢分享
63
谢谢分享.学习了
49
谢谢分享.阅读
57
谢谢分享!
26
好好好好好好好好
24