


























本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

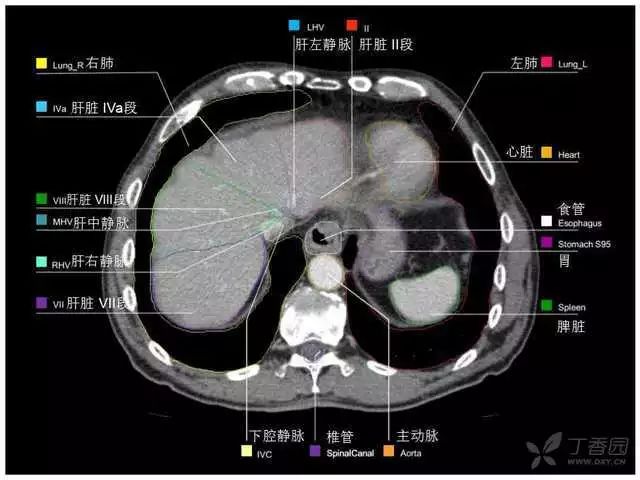
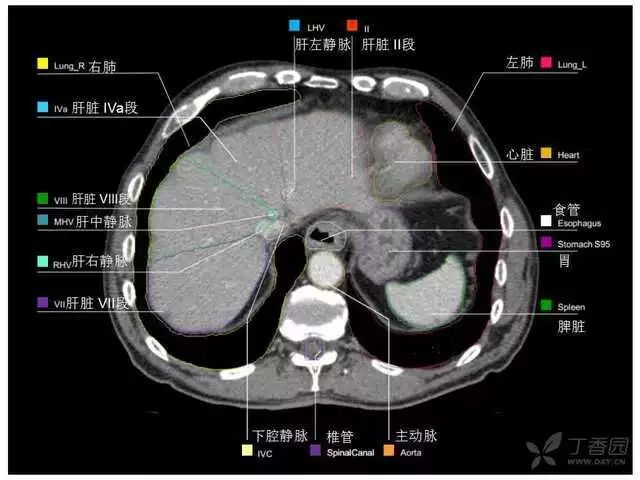
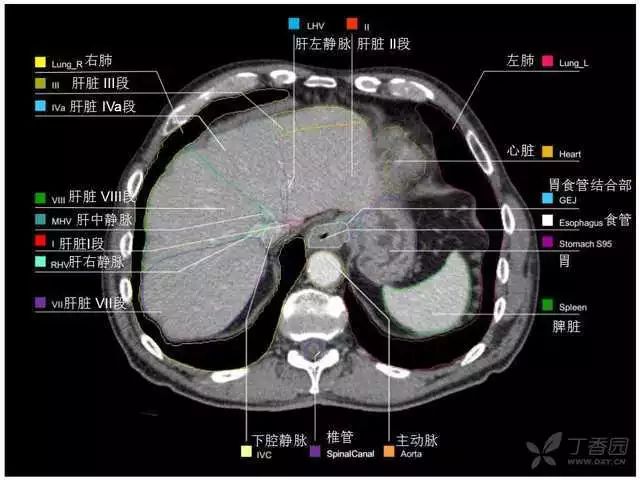
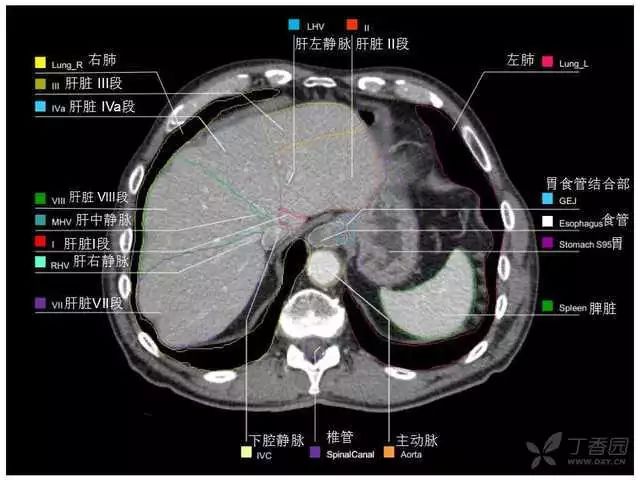
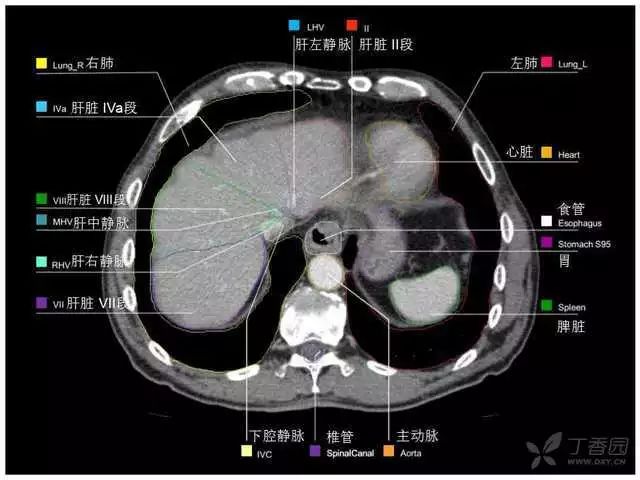
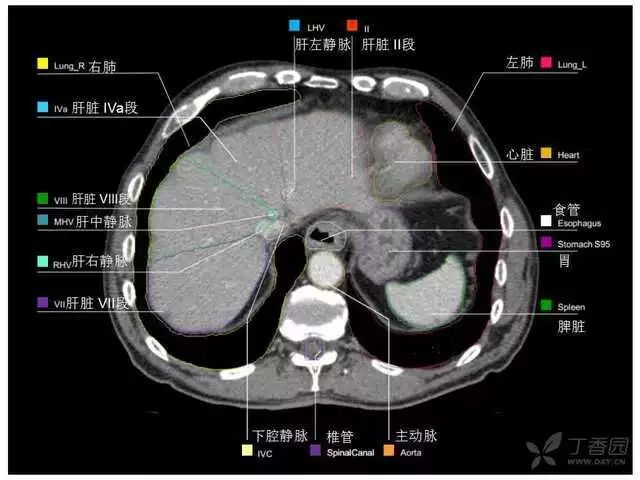
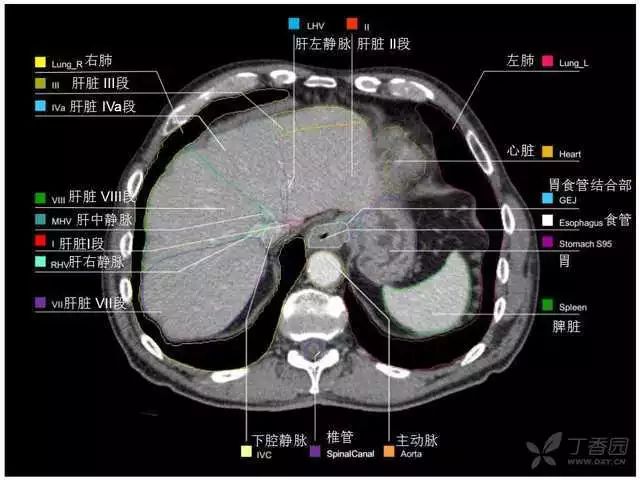
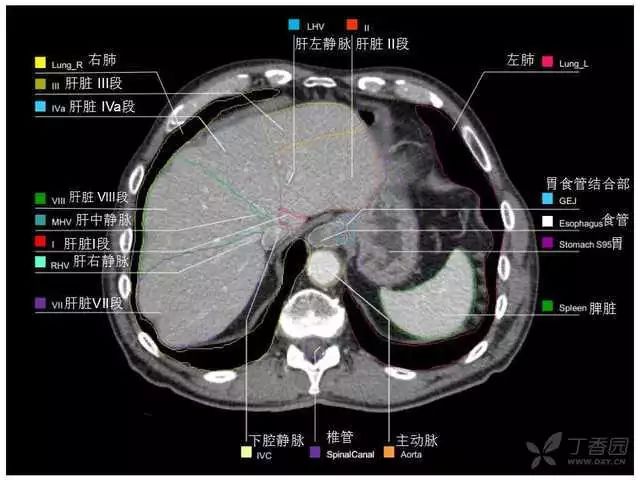
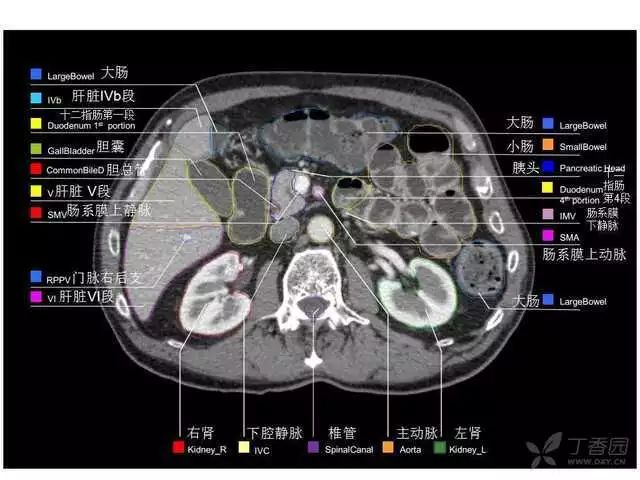
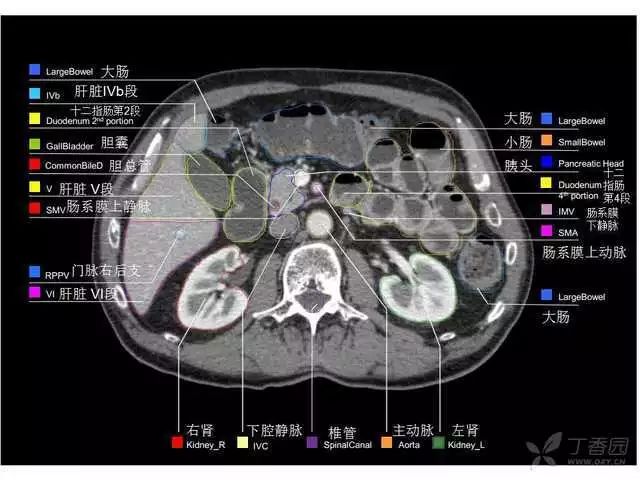
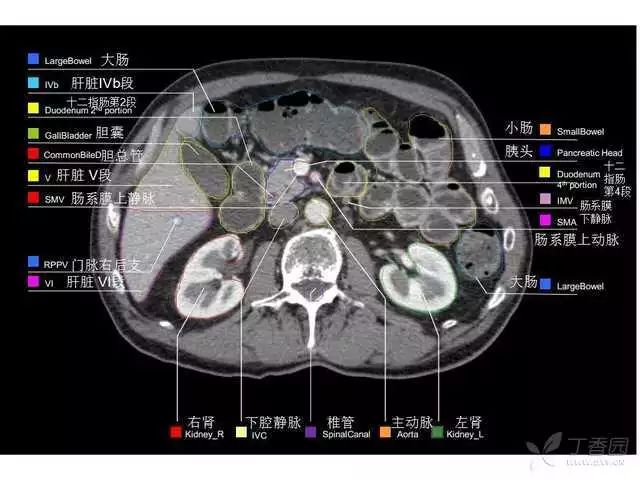
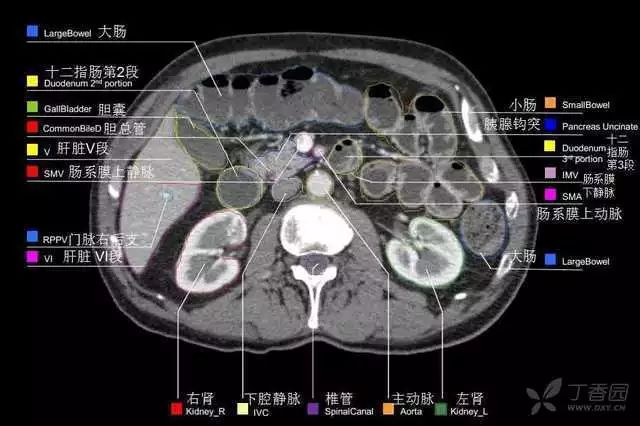
2022-01-30 华夏影像诊断中心 华夏影像诊断中心
太珍贵了,收藏学习!




























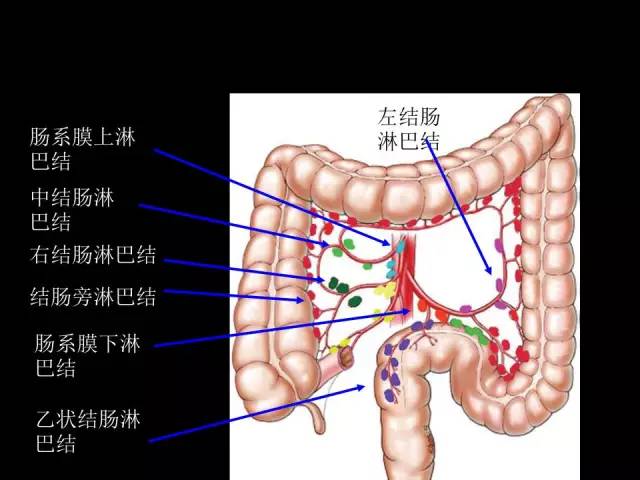
研究认为,小肠神经内分泌肿瘤根治性切除的患者,为获得准确的淋巴结分期至少需要8个淋巴结,存在4个以上淋巴结阳性人群的3年预后变差,彻底的区域淋巴结切除是准确分期和治疗疾病的关键
肿瘤原发灶能够诱导远端转移器官中基质和相关免疫细胞成分与功能变化,形成一个利于肿瘤细胞定居生长“土壤”的 “肿瘤转移前微环境”。
感染这种猴痘菌株的人约有1/100是致命的。然而,对于免疫系统较弱的人来说,感染机率可能更高。
SARS、MERS以及最近的新型冠状病毒2019-nCoV等病原体已成为全球性威胁。淋巴结(LN)通过为免疫细胞的生长提供庇护所并抵抗病原体,从而与传染病作斗争。但是,人们对LN的特定内部运作方式知之甚少。韩国基础科学研究所(IBS)的科学家们发现Hippo-YAP/TAZ信号通路在LN的形成和维持中起主要作用。该研究报告发表在《Nature Communications》杂志上。
生化复发(BCR)前列腺癌(PCa)患者的节点复发挽救性淋巴结清扫(sLND)在当前的指南中仍旧不推荐,主要是由于当前传统成像的不准确性造成。最近,研究人员评估了[68Ga] Ga-PSMA 11 PET(PSMA-PET)在检测PCa淋巴结转移中的表现,并通过sLND进行了病理学确认。研究人员对MEDLINE、SCOPUS、Web of Science和Cochrane Library进行了搜索
韩国基础科学研究所(IBS)的科学家们发现Hippo-YAP/TAZ信号通路在LN的形成和维持中起主要作用。该研究报告发表在《Nature Communications》杂志上。


梅斯医学MedSci APP
医路相伴,成就大医
6666666
31
太实用了,经典
52
学习了,谢谢
66
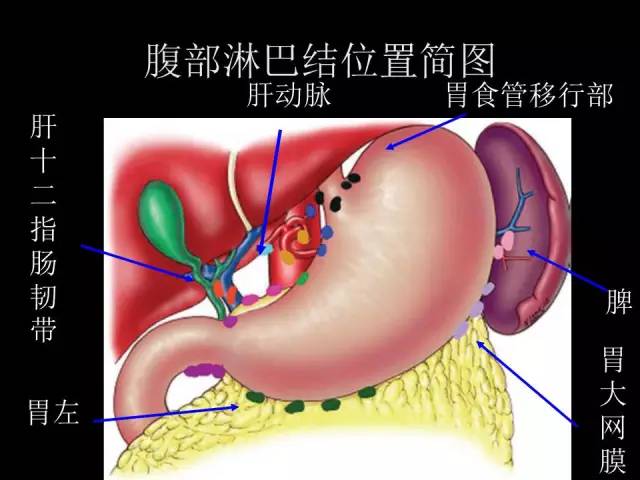
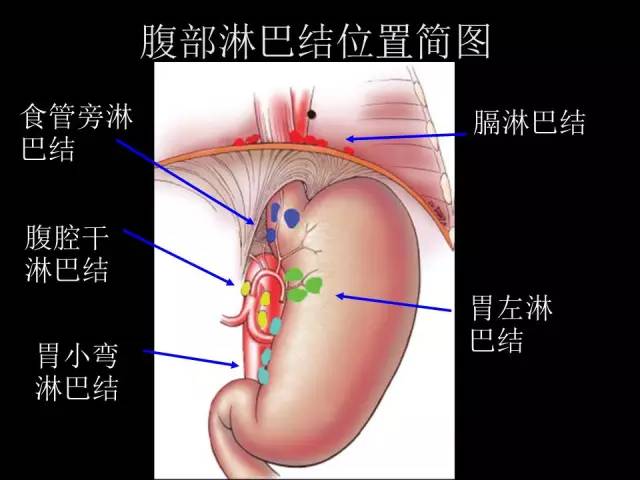
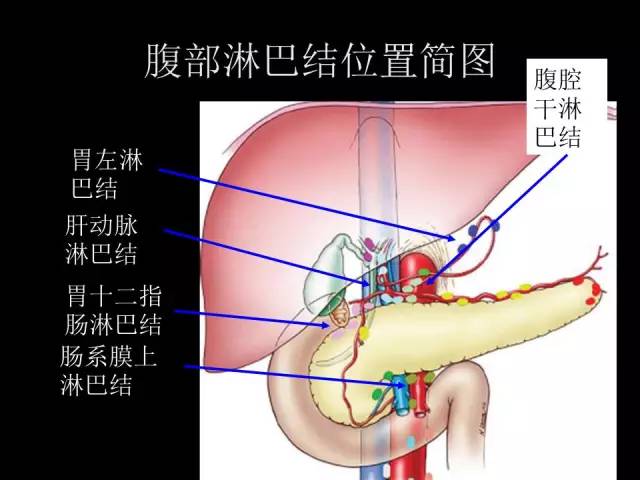
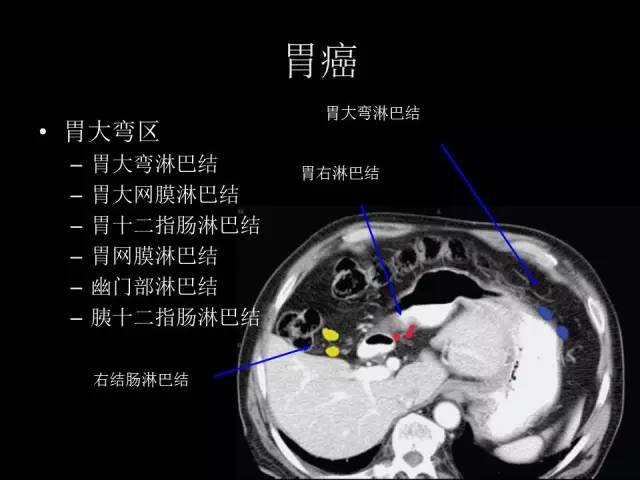
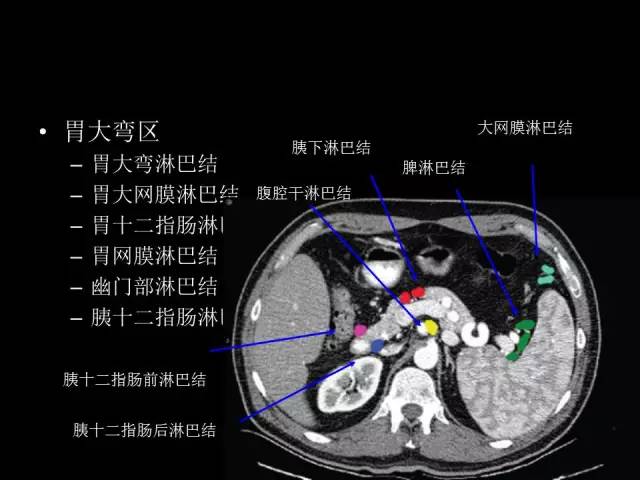
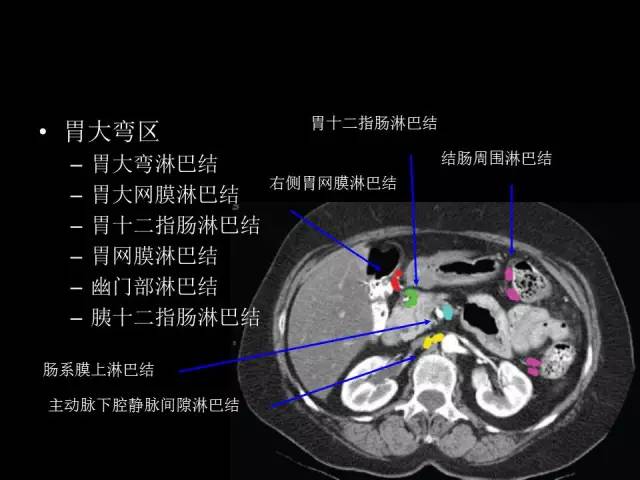
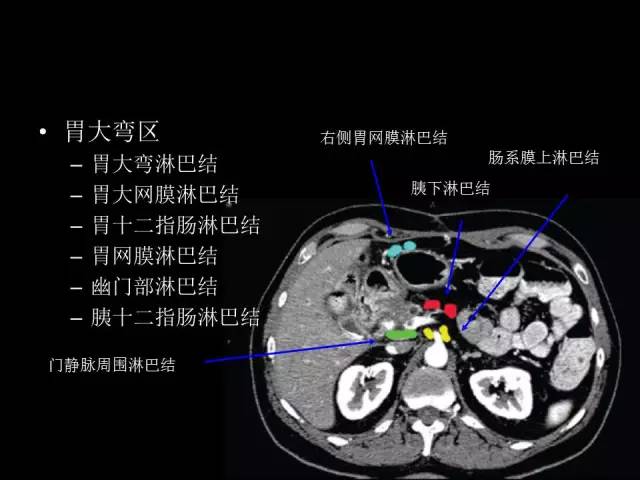
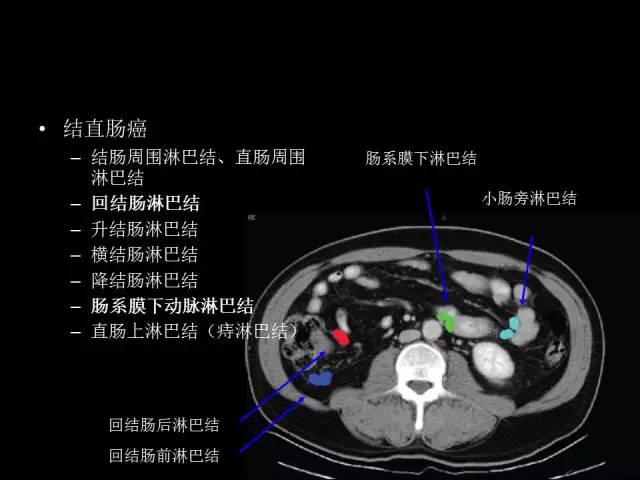
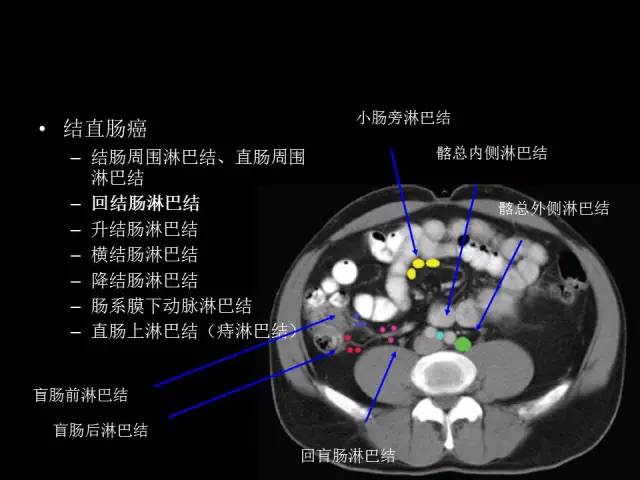
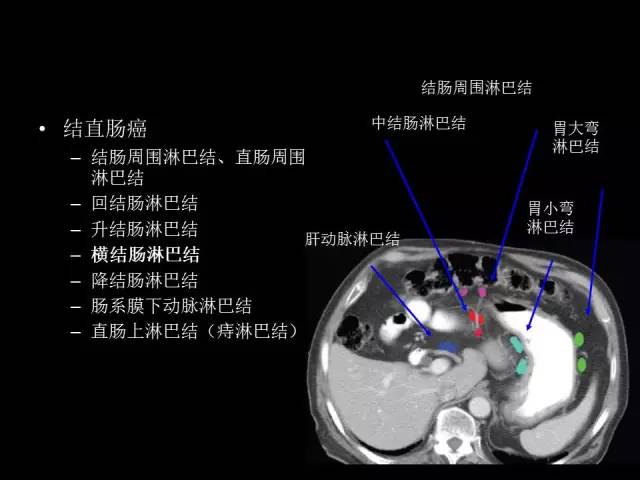
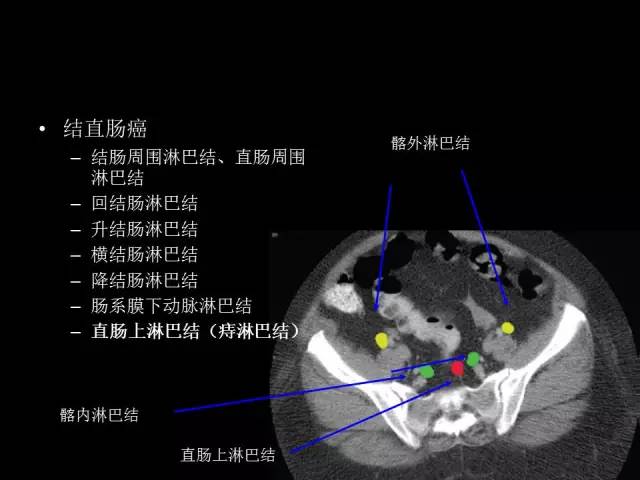
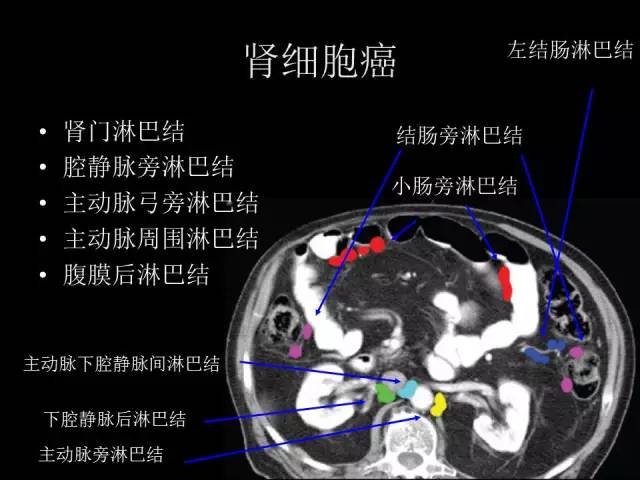
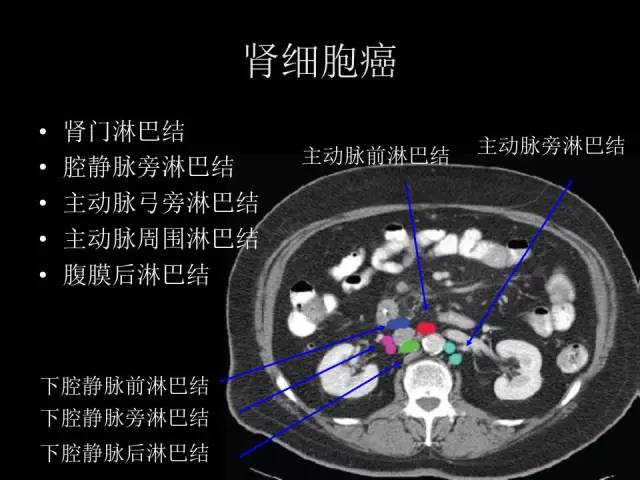
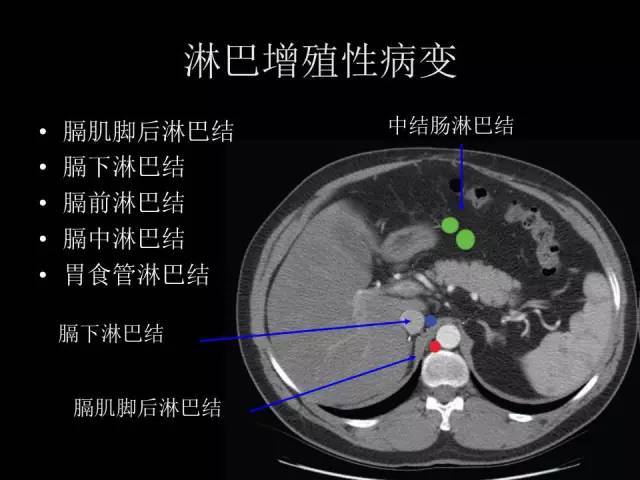
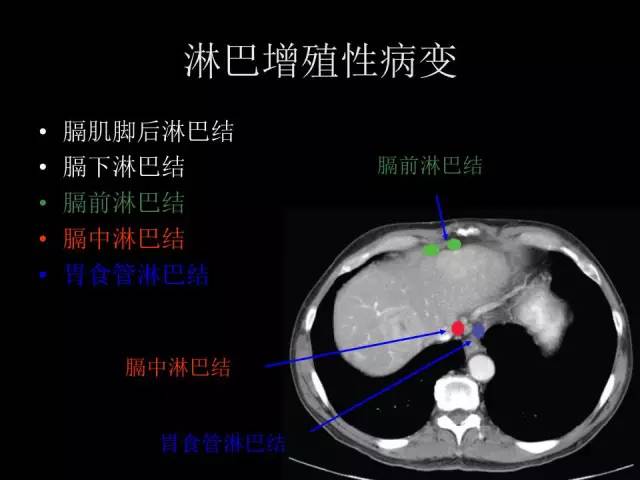
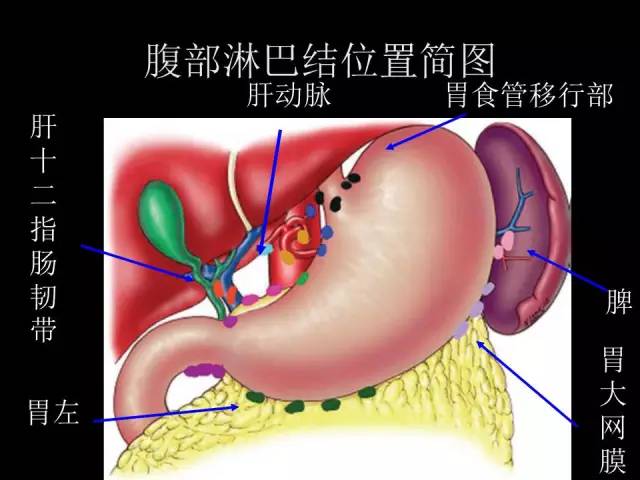
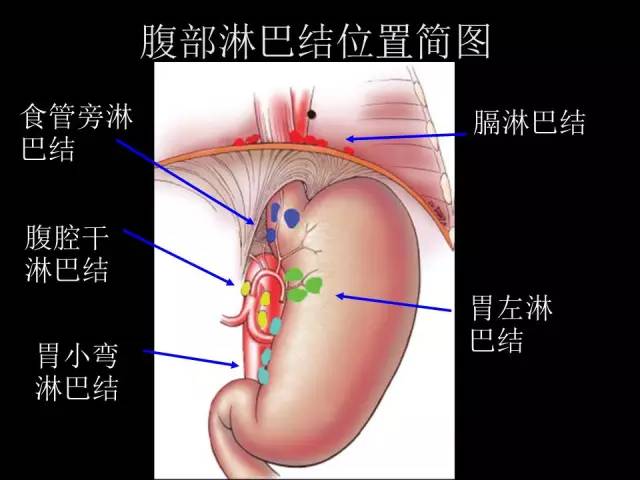
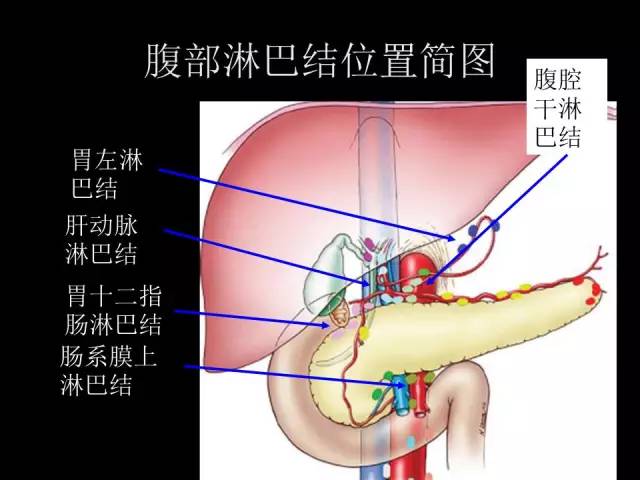
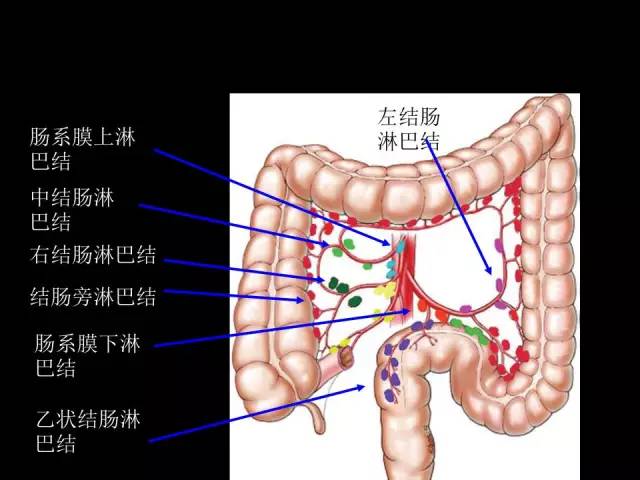
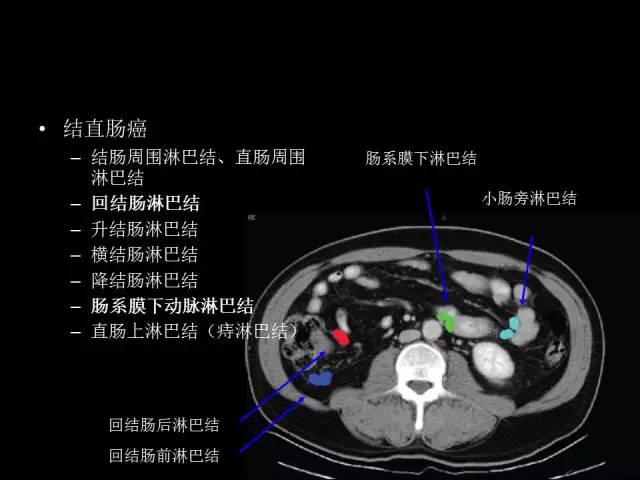
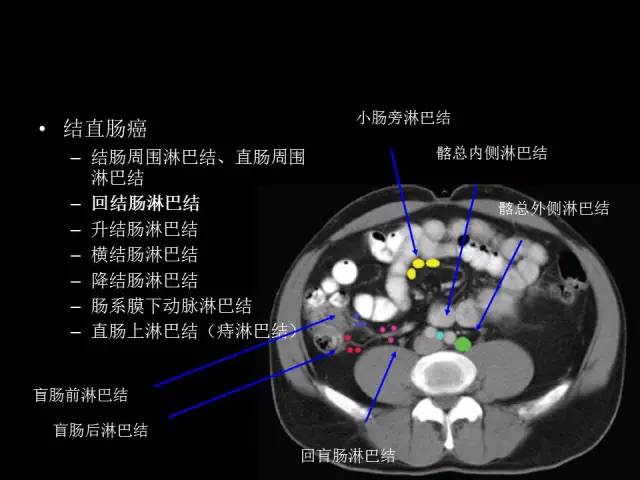
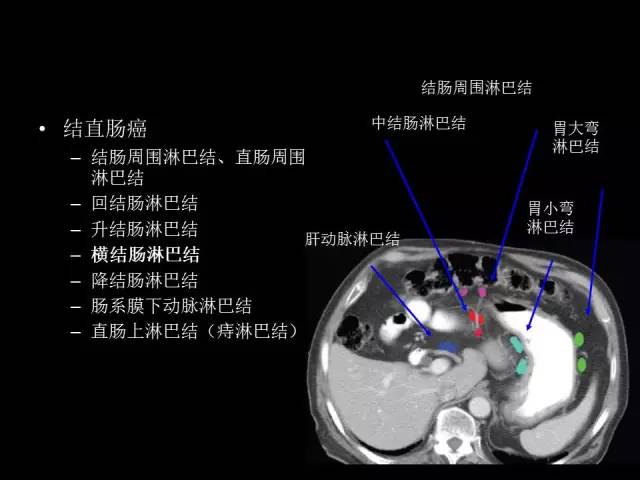
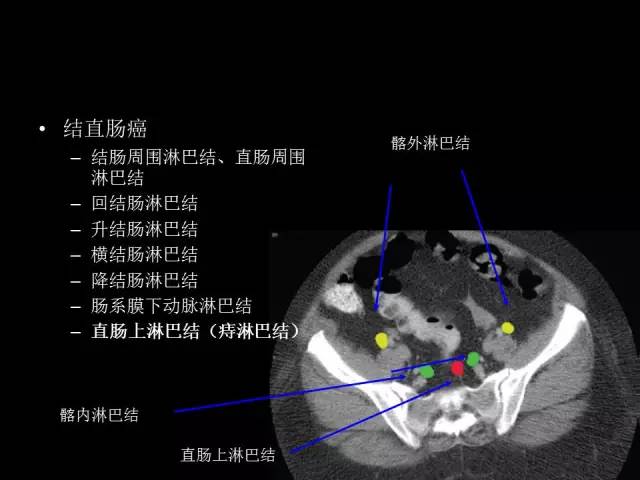
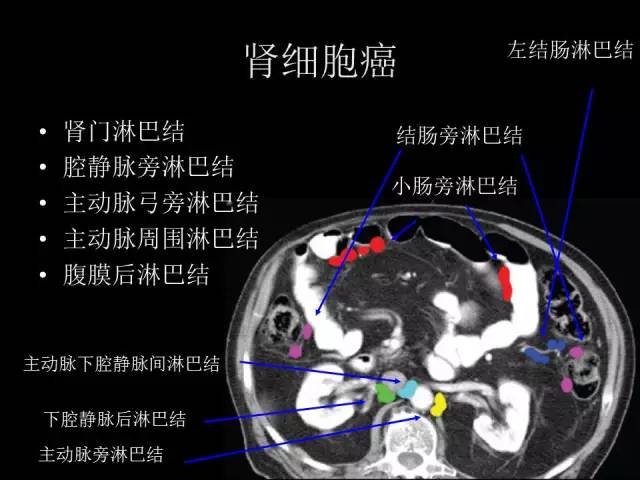
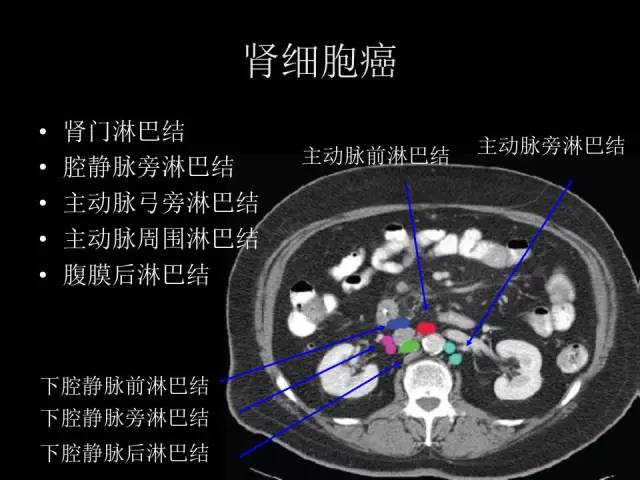
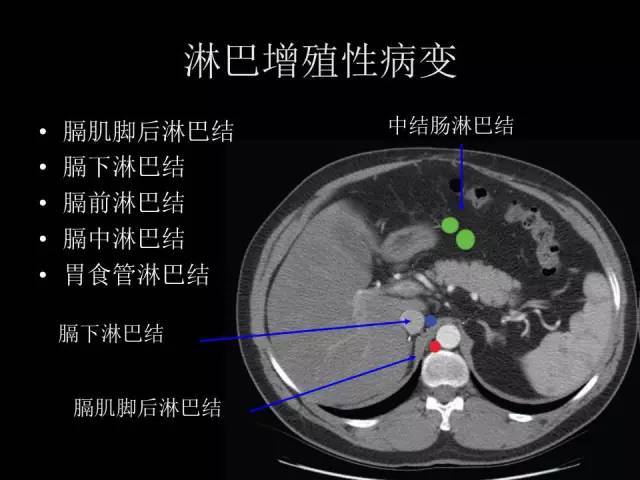
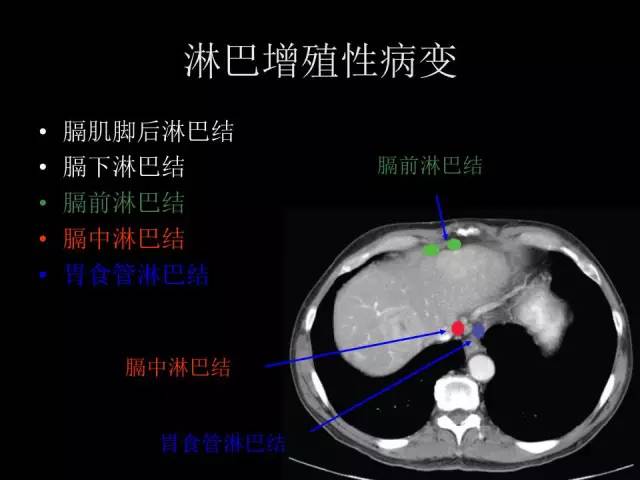
#淋巴结#
65
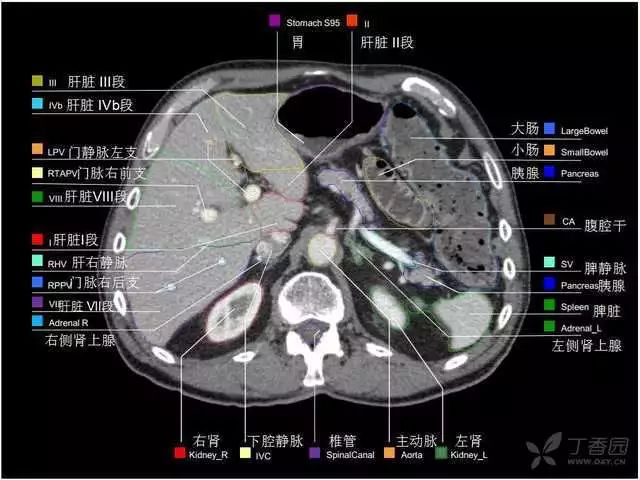
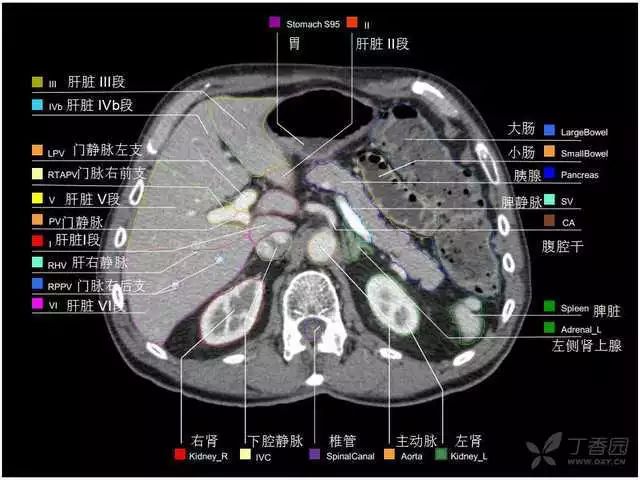
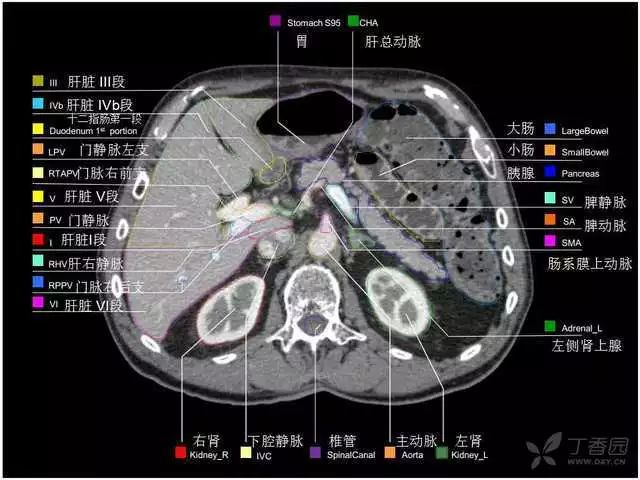
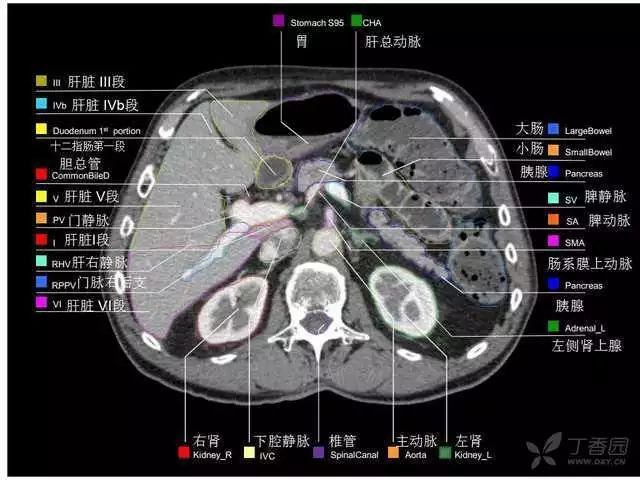
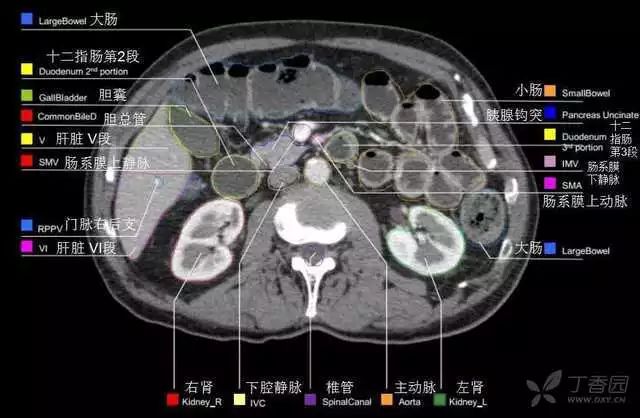
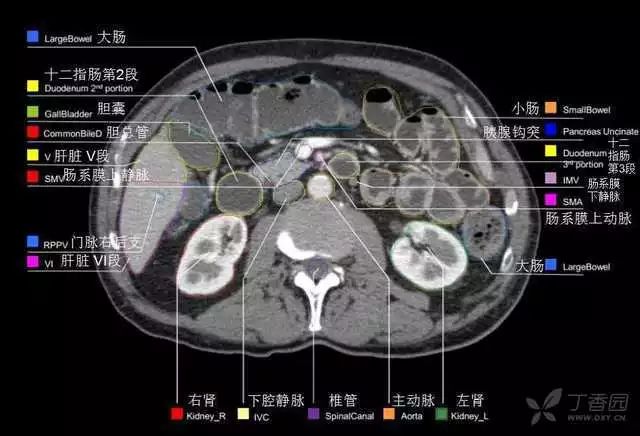
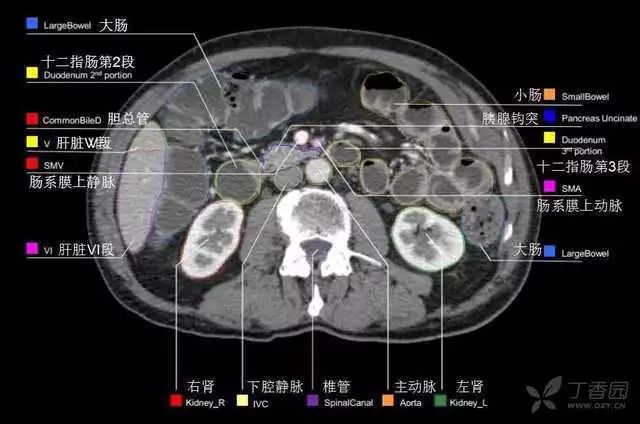
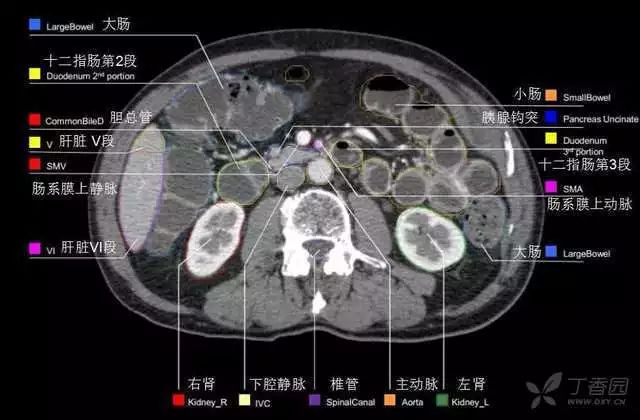
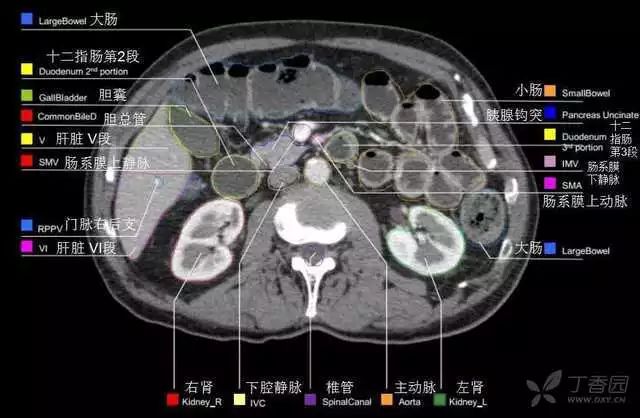
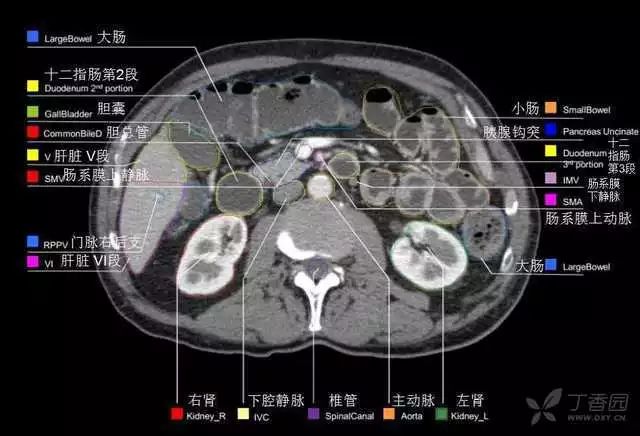
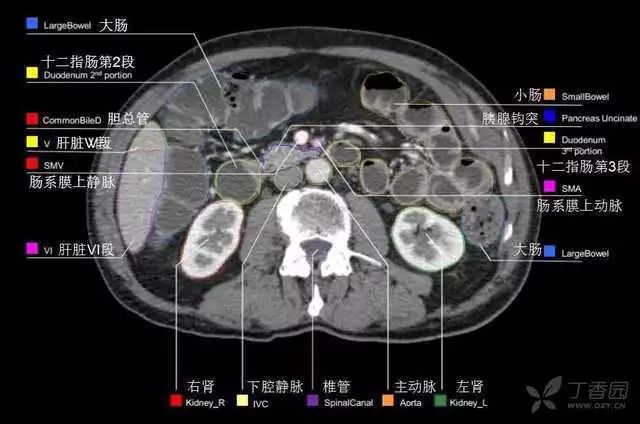
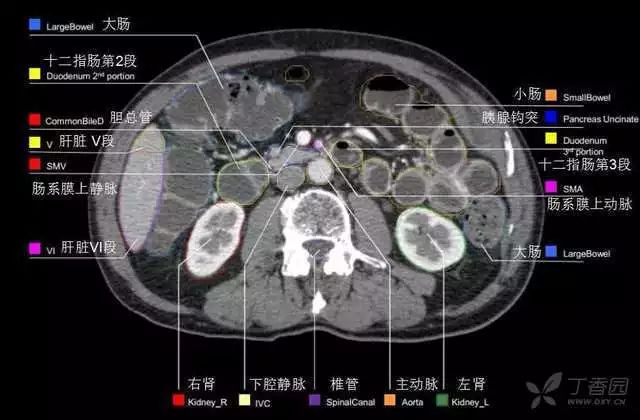
#解剖图#
33
学会了
61
菌感染发生后6-8 h即开始升高,24-48
66
这个很不错!!!
69
学习了,谢谢分享
64