PD-1/IDO组合注册试验开始,小分子IO药物进入三期临床
2016-06-24 佚名 美中药源
Incyte的IDO1抑制剂和默沙东的PD-1抗体Keytruda组合作为一线疗法治疗晚期黑色素瘤的三期临床试验正式开始。这个叫做ECHO301的试验准备招募600病人,按病人PD-L1表达和BRAF变异分成多组,一级终点是无进展生存期和总生存期。试验预计2018年结束。 Keutruda已经是晚期恶黑的一线用药,并且不受BRAF变异限制。而Epacadostat则是最领先的小分子IO药物。二者
Incyte的IDO1抑制剂和默沙东的PD-1抗体Keytruda组合作为一线疗法治疗晚期黑色素瘤的三期临床试验正式开始。这个叫做ECHO301的试验准备招募600病人,按病人PD-L1表达和BRAF变异分成多组,一级终点是无进展生存期和总生存期。试验预计2018年结束。
Keutruda已经是晚期恶黑的一线用药,并且不受BRAF变异限制。而Epacadostat则是最领先的小分子IO药物。二者组合在一期临床中显示57%应答率,这和Keytruda单方50%的应答率类似。但三期临床比较的是无进展生存期和生存期这些对病人更有价值的指标,Epacadostat能带来多少收益还是一个很大的问号。
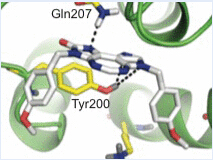
这个实验将是IO疗法的一个重要里程碑。免疫疗法是肿瘤治疗史上的一个关键技术进展,但目前为止都是大分子或细胞疗法的天下。这些疗法都是针对细胞表面受体,而无法直接调控庞大复杂的免疫细胞内免疫应答体系。这个涉及数百个蛋白的调控体系有一些节点可能会和PD-1类似功能或和PD-1抗体有协同作用,而这些靶点最适合用小分子药物调控。
Epacadostat是小分子IO药物先驱,如果显示一定疗效,即使商业上价值有限依然在技术上是个概念验证,会给现在正在早期研究的其它小分子药物一个希望和鼓励。但是和其它IO组合一样,价格将是一个难题。即使在某些特定人群(如PD-L1低表达人群)有统计显着OS改善,但如果改善有限这个组合的定价将面临压力。一是Keytruda已经价格很高,二是IDO抑制剂的长期生存优势需要更多实验证实。因为Keytruda是主要疗效来源,Epacadostat的商业回报或许和其第一个小分子IO药物身份不符。
当然更悲情的结局是作为开拓者的Epacadostat不能改善生存。新药研发教给我们的经验是多数新机理药物会以失败告终,不管我们对它寄予多大希望。PD-1抗体的巨大成功不意味着所有免疫激活剂都能为晚期癌症患者带来深度持久应答。PD-1抗体可能是一个大金矿的一角,也可能就是一个乱石中的一个金块。ECHO301可能ECHO PD-1抗体的颠覆性疗效,也可能ECHO the sound of silence。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#三期临床#
42
#小分子#
35
#IDO#
46
新的希望
133
这个很好
107
感觉很好
98
#注册#
25
#O药#
32