超声心动图“顺藤摸出”多浆膜腔积液病因
2017-07-21 朱天刚 超声心动图与临床决策:疑难病例解析
17岁男性,以胸闷起病,发病前无明显不适症状,胸部X线片提示左侧胸腔积液,抗感染及抽胸腔积液治疗效果不佳,并相继出现双侧胸腔积液、心包积液和腹腔积液。超声心动图结果对本病例最终确诊起到重要指导作用。超声心动图对缩窄性心包炎有何诊断价值? 如何与限制型心肌病的超声心动图鉴别?
17岁男性,以胸闷起病,发病前无明显不适症状,胸部X线片提示左侧胸腔积液,抗感染及抽胸腔积液治疗效果不佳,并相继出现双侧胸腔积液、心包积液和腹腔积液。超声心动图结果对本病例最终确诊起到重要指导作用。超声心动图对缩窄性心包炎有何诊断价值? 如何与限制型心肌病的超声心动图鉴别?
病例摘要
主诉
男性,17岁。主因“间断胸闷2个月”入院。
现病史
患者2个月前无明显诱因出现胸闷,无发热,无咳嗽、咳痰、咯血,无呼吸困难,偶感胸痛,吸气时明显,偶伴夜间盗汗。自觉为上呼吸道感染,口服相关药物后症状无缓解,当地县医院X线胸片提示左侧胸腔积液,给予抗感染和胸腔穿刺抽吸胸腔积液治疗效果不佳,并相继出现对侧胸腔积液、心包积液、腹腔积液伴双下肢水肿。为求进一步诊治收入我院呼吸科。
既往史
个人史
出生及生长于河北,学习、生活环境良好。无特殊粉尘、放射线接触史。吸烟史1年,5~6支/日。否认饮酒史。
家族史
父母体健。否认家族遗传性疾病史。
体格检查
体温37.0℃,脉搏100次/分,呼吸18次/分,血压120/90mm Hg。发育正常,营养良好。全身浅表淋巴结未触及肿大。眼睑略水肿。颈静脉充盈,无颈动脉异常搏动。气管居中,甲状腺无肿大。胸廓对称,无畸形。双肺叩诊浊音,双肺呼吸音粗,双下肺呼吸音减弱,未闻及干、湿啰音。心前区无异常隆起或凹陷,心界叩诊不大,心率100次/分,律齐,各瓣膜区未及明显杂音。腹部平坦,肝肋下2指,腹部叩诊鼓音,移动性浊音可疑阳性,肠鸣音4次/分。双下肢无水肿。无杵状指。
辅助检查
血常规、肝功能、肾功能、甲状腺功能正常。自身免疫抗体阴性。胸腔积液检查:胸腔积液介于漏出液、渗出液之间。X线胸片:左侧胸腔积液,心影无异常。胸膜活检病理未见肿瘤。心电图:窦性心动过速,ST-T改变。腹部超声:慢性肝淤血,胆囊壁水肿,双侧胸腔积液,腹腔积液。门诊超声心动图:轻度二尖瓣、三尖瓣反流,微量心包积液。
初步诊断
多浆膜腔积液原因待查,结核性胸膜炎?自身免疫性疾病?恶性胸腔积液?
诊疗经过
根据实验室检查结果,考虑肝源性、肾源性、甲状腺功能减低、自身免疫性疾病以及肿瘤所致多浆膜腔积液病因可基本排除。门诊初次超声心动图未发现可解释多浆膜腔积液的病变,但既往当地医院胸部CT可见心包不规则增厚,因此建议复查超声心动图,以明确有无缩窄性心包炎,确定下一步治疗方案。
入院后,复查超声心动图:①心包不规则增厚、回声增强,以左心室侧壁、左心室后壁、左心室下壁和右心室侧壁处明显,最厚处达8mm(图86-1 A);②室间隔运动异常,吸气时向左心室侧偏移(图86-1A、86-1B);③双心房轻度扩大,左心室壁、右心室壁舒张受限;④二尖瓣舒张期血流频谱E/A>1,E峰速度随呼吸相变化,吸气时下降约32%(图86-1C);⑤下腔静脉增宽,近心段内径约21mm,内径不随呼吸相变化(图86-1D),肺静脉增宽,右上肺静脉入口处内径约10mm(图86-1E);⑥脉冲组织多普勒二尖瓣环室间隔舒张早期速度E'较高,约10cm/s(图86-1F)。结论:考虑缩窄性心包炎可能性大。
依据超声心动图结果,考虑缩窄性心包炎诊断成立。鉴于我国缩窄性心包炎患者的最常见病因为结核感染,征得患者及家属同意后给予诊断性抗结核药物治疗。并请心外科医生会诊,建议转至心外科行手术治疗。患者在全麻下接受心包切除术,术中可见心包不规则增厚 (最厚处约1cm),心包脏层与壁层粘连、纤维化,未见心包腔积液。心包病理学检查:上皮样肉芽肿炎,可见朗格汉斯巨细胞及干酪样坏死,抗酸 (+), PAS(-),考虑结核。术后患者恢复较好,出院继续抗结核药物以及强心、利尿等抗心力衰竭治疗。
最终诊断
缩窄性心包炎,多浆膜腔积液。
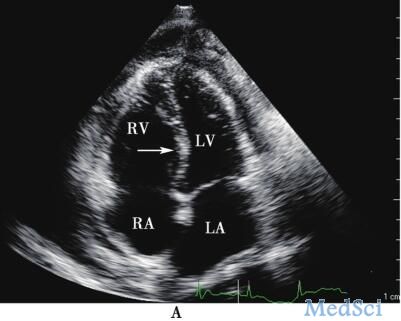
图86-1 入院超声心动图 A:心包不规则增厚、回声增强,室间隔吸气时向左心室侧运动 (箭头所示)

B:M型超声心动图显示室间隔运动异常,吸气时室间隔偏移向左心室侧

C:频谱多普勒显示二尖瓣舒张期E峰速度于吸气时下降32%
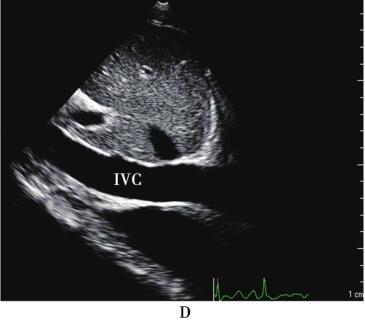
D:剑下切面显示下腔静脉增宽,内径不随呼吸运动改变
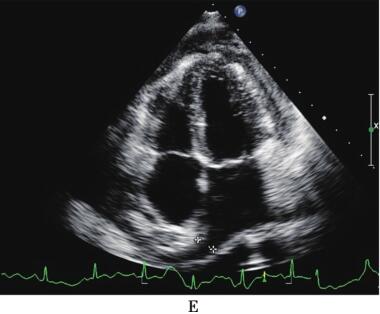
E:显示肺静脉增宽
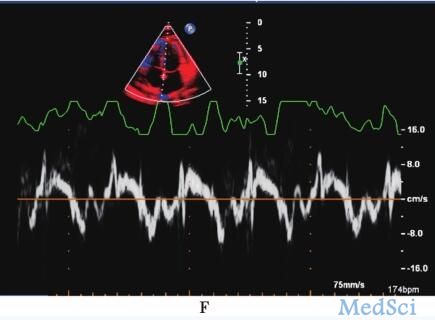
F:脉冲组织多普勒显示二尖瓣环室间隔舒张早期速度E'约10cm/s。LA:左心房;LV:左心室;RA:右心房;RV:右心室;IVC:下腔静脉
病例思考
1.本例患者的临床特点、超声心动图表现是什么?
本例患者为青年男性,以胸闷起病,发病前无明显不适症状,胸部X线片提示左侧胸腔积液,抗感染及抽胸腔积液治疗效果不佳,并相继出现双侧胸腔积液、心包积液和腹腔积液。实验室检查提示肝功能、肾功能、甲状腺功能正常,自身免疫抗体阴性,胸膜活检未见肿瘤。综合患者病史、辅助检查,临床考虑心包疾病可能性较大。
门诊超声心动图虽无病因学提示,但入院后复查超声心动图显示心包不规则增厚、回声增强,室间隔运动异常,双心房轻度扩大,心脏舒张受限,考虑缩窄性心包炎(constrictive pericarditis,CP)可能性大。超声心动图结果对本病例最终确诊起到重要指导作用。
2.缩窄性心包炎的病理生理机制是什么?
缩窄性心包炎是心包慢性炎症导致心包增厚、粘连、纤维化甚至钙化,使心脏在舒张期充盈受限,引起全身血液循环障碍的疾病。引起缩窄性心包炎的原因包括感染、结缔组织病、肿瘤、机械创伤、心内直视手术或纵隔放疗等,我国患者的最常见病因为结核感染。缩窄性心包炎患者可因心包纤维化、钙化压迫心脏,使各心腔舒张期充盈受限,体循环、肺循环回流受阻,导致舒张期血容量减少、心排出量减低。主要临床症状、体征为严重慢性体循环、肺循环淤血伴低心排出量表现,多数患者并无急性期表现。
3.缩窄性心包炎的诊断方法与确诊依据是什么?
缩窄性心包炎通常起病隐匿,首发表现可涉及多个脏器系统,缺乏特异性,易被临床医生漏诊、误诊或诊断滞后,因此早期确诊一直是临床难题。
心电图无特异性改变,常可见QRS波低电压、ST-T改变和房性心律失常。X线胸片可表现为左右心缘变直、上腔静脉增宽和胸腔积液等征象,偶可见心包钙化。心脏CT与MRI均可准确测量心包厚度。其中,CT对于显示心包增厚、钙化灶具有明显的优势,但不能动态显示心脏舒张受限情况及血流动力学改变。一般观察到心包钙化有助于确诊缩窄性心包炎,但个别病例可能有心包钙化而无心包缩窄的功能改变,因此必须结合临床及其他征象。有创的心导管检查可有特异性表现,即心室舒张期压力曲线呈平方根样,左心室、右心室舒张末期压差≤5mm Hg。无创性超声心动图对缩窄性心包炎诊断具有重要价值。
4.超声心动图对缩窄性心包炎有何诊断价值?
超声心动图是无创、便捷的诊断技术,能够实时、直观显示心包和心脏的形态学改变,多普勒超声心动图可评估心脏血流动力学变化,常规及组织多普勒等新技术能够评价整体、局部心肌功能,因此对诊断与鉴别诊断缩窄性心包炎起着举足轻重的作用,并可为制订治疗策略发挥关键作用。另外,超声心动图还能够鉴别缩窄性心包炎与限制型心肌病,二者临床表现十分相似,但病因、治疗方法和预后完全不同。具体而言,缩窄性心包炎的超声心动图诊断要点包括:
二维、M型超声心动图:①心包增厚、回声增强,尤以房室沟处显着;②心房扩大,心室相对较小;③左心室、右心室舒张受限;④室间隔运动异常,舒张早期反常向左心室内摆动并可立即回弹;⑤下腔静脉、肝静脉和肺静脉增宽,提示体循环、肺循环淤血。
多普勒超声心动图:①心室充盈的呼吸性变化,吸气时二尖瓣E峰流速下降超过25%;②二尖瓣血流频谱表现为“限制型”充盈,E/A>1.5,E峰减速时间<150ms。
5.如何与限制型心肌病的超声心动图鉴别?
限制型心肌病是由于心内膜、心肌病变 (如纤维化)导致心室充盈受限和心室舒张功能障碍的一类心肌病。而缩窄性心包炎的基本病理生理改变是心包压迫心脏,使其充盈受限和心室间依赖性增高,多数患者心肌收缩、舒张功能并无特殊异常。超声心动图除可完成形态学评估外,还能无创评价血流动力学、心肌功能,实现对两种疾病的有效鉴别诊断。主要鉴别要点:限制型心肌病患者的超声心动图一般无明显心包增厚;心房扩大更为显着;无室间隔的异常运动;吸气相二尖瓣E峰流速变化<15%;二尖瓣环E'通常明显减低,E/E'常大于15;肺动脉压增高更明显。
病例启示
遇到有心包积液病史和体循环、肺循环淤血体征的患者,超声心动图医生既应详尽观察心包厚度、回声,尤其房室沟处心包情况,还需仔细观察有无心室充盈受限和心室间依赖性增高变化,如室间隔异常运动,呼吸性漂移,二尖瓣、三尖瓣E峰速度随呼吸变化,下腔静脉、肺静脉扩张等。如有上述典型特征,均提示缩窄性心包炎诊断。超声心动图诊断缩窄性心包炎还需注意以下问题:
1.区别心包增厚与心包缩窄
心包增厚并非一定为缩窄性心包炎,也可见于急性心包炎患者,多因心包膜肿胀、渗出及纤维素附着导致心包增厚,但随着病程好转,渗出液及纤维素吸收后,心包膜可完全恢复正常。另外有部分缩窄性心包炎患者心包厚度正常。鉴别关键是评价心脏是否出现缩窄性心包炎所致的形态学、血流动力学改变。
2.心包缩窄是否为一过性
7%~10%急性心包炎可见一过性缩窄期,因此要注意超声心动图随访。
3.是否为渗液性-缩窄性心包炎
据报道,24%缩窄性心包炎为渗液性-缩窄性心包炎,检查时要注意探查有无心包腔液性无回声区。
4.有何超声心动图线索
超声心动图需尽量为临床医生提供更多诊断信息,包括心包增厚特征、位置,室间隔异常活动,肺静脉、肝静脉血流方向等定性资料,以及最大心包厚度,二尖瓣E/A、E峰减速时间,二尖瓣、三尖瓣血流随呼吸变化程度,E/E'以及下腔静脉内径/塌陷指数等定量数据。
5.超声心动图漏诊原因分析
①忽视临床资料,对缩窄性心包炎缺乏警惕;②对缩窄性心包炎的血流动力学改变、相应超声表现理解欠深刻;③缩窄性心包炎缺乏特异性诊断指标。
来源:《超声心动图与临床决策:疑难病例解析》
作者:朱天刚
参编:丁 茜 权 欣 王 欣 丁文虹 马 为
页码:404-408
出版:人民卫生出版社
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#心动图#
37
#浆膜腔积液#
35
学习了谢谢分享
64
学习了谢谢分享
61
学习了谢谢分享
59
henhao
43
学习学习
72