Hypertension:纵向血压变化与慢性肾脏疾病进展的关系
2021-11-03 从医路漫漫 MedSci原创
在慢性肾脏疾病(CKD)患者中,血压(BP)升高是很常见的,并认为是进展到终末期肾病(ESKD)、心血管疾病和死亡的主要危险因素。
在慢性肾脏疾病(CKD)患者中,血压(BP)升高是很常见的,并认为是进展到终末期肾病(ESKD)、心血管疾病和死亡的主要危险因素。肾功能逐渐减退时通过交感神经系统过度活跃、肾素-血管紧张素-醛固酮系统和钠潴留导致血压升高。因此,除其他常规措施外,控制血压是糖尿病患者保护肾脏的主要治疗措施,包括减少尿蛋白排泄、限制饮食盐和蛋白质摄入、戒烟、充分控制血糖等。关于BP的纵向时间变化趋势及其对肾功能影响的研究尚不多见。在这里,我们评估了收缩压(SBP)随时间变化的动态变化与不利肾脏预后的关系。
方法:该KNOW-CKD是一项涉及韩国非透析CKD患者的全国性前瞻性队列研究。2011年至2016年,来自9家三级医院的2238名参与者被纳入研究,并随访至2019年3月31日。在2238名参与者中,我们排除了以下患者,因为他们的血压变化无法确定:(1)55名患者只进行了基线检查,此后未进行随访;(2) 95例无基线血压或实验室资料;(3) 105例暴露期间无血压值记录;(4)81例随访时间<1年;(5) 65例患者在基线随访后1年内出现主要预后。最终,1837例患者被纳入分析。为了对BP随时间变化的趋势进行分类,我们应用了基于分组的变化建模。利用这种有限混合建模方法,将纵向BP数据拟合为多个潜在轨迹的混合,并采用时间多项式的截尾正态模型进行拟合。最后,我们确定了3个不同的SBP变化趋势: 268例(14.5%)、1211例(65.9%)和358例(19.5%)患者分别被分为收缩压降低组、收缩压稳定组和收缩压升高组。在0、6和12个月的3次SBP测量中确定。主要结果是CKD进展,定义为估算的肾小球滤过率较基线值或终末期肾病发生的复合结果。
结果:收缩压降低组的收缩压从144mmHg下降到120mmHg,收缩压升高组的收缩压在1年内从114mmHg上升到136mmHg。在6576人年的随访中(中位数,3.7年) ,综合结果发生在521名(28.4%)参与者。收缩压降低组(30.6%)和稳定组(26.5%)的主要预后事件明显少于收缩压升高组(33.0%)。在多变量调整的特定原因危险模型中,与稳定的SBP相比,收缩压增加与不良肾脏结局风险增加1.28倍相关。然而,收缩压下降和稳定组的主要预后风险没有差异。
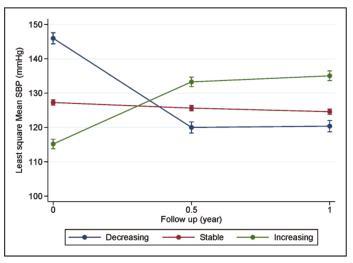
图1 根据收缩压观察一年内收缩压变化趋势。
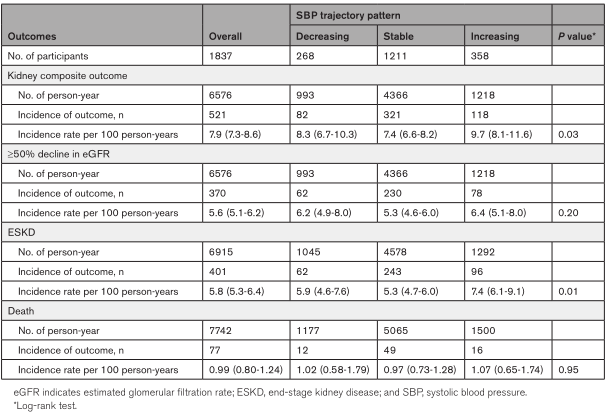
表1 根据收缩压变化的结局事件率
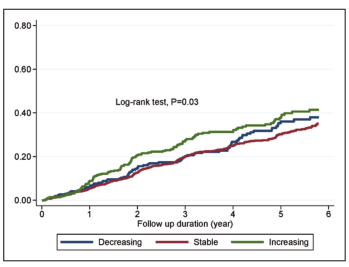
图2 根据收缩压变化的肾脏不良结局累积发生率曲线;不良肾脏结局定义为在随访期间估计肾小球滤过率(eGFR)较基线值下降≥50%或终末期肾病发病的复合结果。

表2 根据收缩压变化对综合结局的Cox HR分析
结论:在这项纵向CKD队列研究中,与收缩压稳定相比,收缩压升高组与不良肾脏结局的高风险相关,而收收缩压降低则表现出类似的风险。
原文出处:
Joo YS, Kim HW, Nam KH,et al.Association Between Longitudinal Blood Pressure Trajectory and the Progression of Chronic Kidney Disease: Results From the KNOW-CKD.Hypertension 2021 Aug 15
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血压变化#
52
#PE#
42
#TENS#
45
#疾病进展#
36
#Hypertension#
36
#慢性肾脏#
46
不错
56
谢谢分享
58
谢谢分享
50