Stroke:基底动脉有钙化会影响后循环大血管闭塞后血栓切除手术预后吗?
2020-06-27 shaosai MedSci原创
前循环脑卒中患者颈内动脉颅内段钙化与血管内血栓切除手术预后较差具有相关性。本研究旨在评估后循环大血管闭塞患者椎基底动脉钙化(VBAC)与行血管内血栓切除手术预后的相关性。
背景与目的
前循环脑卒中患者颈内动脉颅内段钙化与血管内血栓切除手术预后较差具有相关性。本研究旨在评估后循环大血管闭塞患者椎基底动脉钙化(VBAC)与行血管内血栓切除手术预后的相关性。
方法
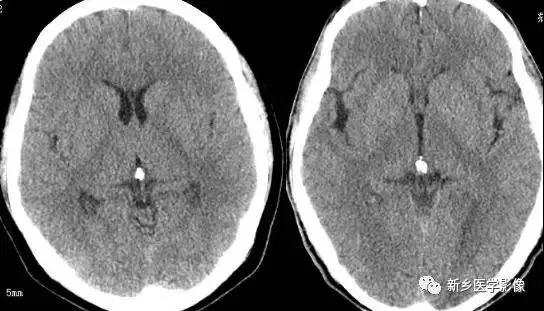
本研究纳入了后循环大血管闭塞并接受治疗的患者。在CT图像上对VBAC进行手动分割。利用倾向性评分logistic回归分析比较VBAC、VBAC体积、功能性恢复(90天mRS评分为0-2分)及90天死亡率的相关性。
结果
本研究共纳入了64例后循环大血管闭塞的患者。共有25例(39.1%)患者具有VBAC,其中VBAC体积中位数为19.8 (6.65-23.4) mm3。VBAC与功能性恢复率降低(OR, 0.19 [95% CI, 0.04-0.78]; P=0.03)、死亡率升高(OR, 9.44 [95% CI, 2.43-36.62]; P=0.005)具有相关性。VBAC体积越大是功能性恢复率降低、死亡率升高的独立预测指标。
结论
本研究表面VBAC是后循环大血管闭塞患者行血栓切除手术预后的独立预测指标。考虑到VBAC的出现时预测术后风险的指标,在临床决策时应十分慎重。
原始出处:
Diprose WK, Diprose JP, Tarr GP et al.Vertebrobasilar Artery Calcification and Outcomes in Posterior Circulation Large Vessel Occlusion Thrombectomy.DOI: 10.1161/STROKEAHA.119.027958
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#大血管#
37
#血管闭塞#
49
#血栓切除#
58
#切除手术#
41
#基底动脉#
43