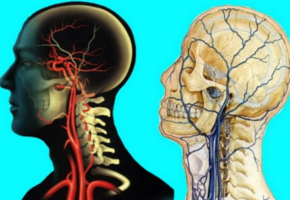
Stroke:皮层静脉充盈是大脑中动脉卒中患者临床预后的预测因子
2016-05-25 MedSci MedSci原创
背景:闭塞动脉的下游的静脉血流可影响缺血性卒中患者的预后。研究者旨在应用动态CT血管造影评估皮层静脉充盈(CVF)情况,并且评估其与临床预后的关系。方法:大脑中动脉近端闭塞患者在卒中发病后9小时内行CT平扫及全脑CT灌注/动态CT血管造影。研究者定义不良预后为改良Rankin量表评分≥3。应用泊松回归分析CVF范围和速率和3个月不良预后的相关性。除外年龄,卒中的严重程度、治疗方式、ASPECT评分
背景:闭塞动脉的下游的静脉血流可影响缺血性卒中患者的预后。研究者旨在应用动态CT血管造影评估皮层静脉充盈(CVF)情况,并且评估其与临床预后的关系。
方法:大脑中动脉近端闭塞患者在卒中发病后9小时内行CT平扫及全脑CT灌注/动态CT血管造影。研究者定义不良预后为改良Rankin量表评分≥3。应用泊松回归分析CVF范围和速率与3个月不良预后的相关性。除外年龄,卒中的严重程度、治疗方式、ASPECT评分、脑血流量和侧枝循环外,应用Logistic回归分析最佳CVF(皮层静脉最大充盈区),并计算曲线下面积。
结果:共有88例患者纳入研究,平均年龄67岁。将最佳CVF范围和速度结合分析,研究者观察到最佳CVF良好并且较快的患者,不良预后风险下降,风险比为0.5(95%CI,0.3-0.7)。与没有纳入CVF的风险模型相比,最佳CVF的范围和速率预测价值增加(曲线下面积为0.88;95%CI,0.77-0.98)。
结论:CT血管造影评估中, CVF的范围和速度结合可用于识别大脑中动脉卒中患者3个月临床预后差的高风险患者。
原始出处:
van den Wijngaard IR, Wermer MJ, et al. Cortical Venous Filling on Dynamic Computed Tomographic Angiography: A Novel Predictor of Clinical Outcome in Patients With Acute Middle Cerebral Artery Stroke. Stroke. 2016 Mar.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#静脉#
46
#大脑中动脉#
49
#卒中患者#
31
拜读了,受益匪浅,点个赞!
73
#皮层静脉充盈#
45
#预测因子#
32
#临床预后#
37