Neurology:奥克立珠单抗Ocrelizumab,治疗进展性多发性硬化,安全性如何?
2021-09-06 Freeman MedSci原创
在临床试验中连续服用OCR长达7年,以及在现实世界中更广泛地使用OCR超过3年,都与良好的和可管理的安全状况有关,在异质性MS人群中没有出现安全问题。
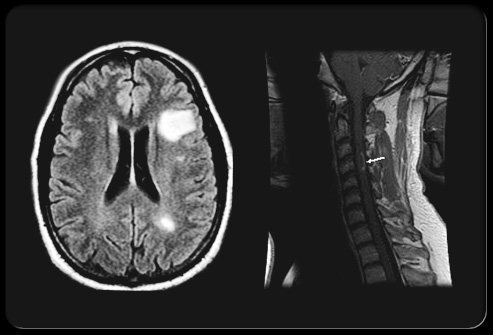
奥克立珠单抗(OCR)是一种重组的人源化单克隆抗体,可选择性地清除表达CD20的B细胞,同时保留B细胞重组的能力和原有的体液免疫力。
这些试验的结果显示,OCR与干扰素(IFN)β-1a或安慰剂相比,几乎完全抑制了新的大脑MRI活动,明显减少了残疾进展,并且与IFNβ-1a相比,复发活动明显降低。OCR的临床益处在长达7年的随访期间被证明是持续的,在较早开始OCR治疗的患者中,有更有利的残疾结果。
在关键的3期试验的控制治疗期(CTPs),输液相关反应(IRRs)、呼吸道感染和尿路感染(UTIs)是与OCR相关的最常见的不良事件(AEs)。
在接受OCR治疗的患者中,相对于其参照物,观察到恶性肿瘤的数量不平衡,主要是由较高的乳腺癌比率所驱动;总体而言,这些事件并不常见。因此,为了解OCR在多发性硬化症患者(patients with MS;PwMS)中的长期获益-风险状况,需要进行安全监测。
藉此,加州大学洛杉矶分校的dStephen L Hauser等人,对11项临床试验中使用OCR治疗的PwMS进行了综合的安全性分析。截至2020年1月,在长达7年的时间里,使用OCR治疗的PwMS的综合安全性分析,并报告了全球上市后监测的特别评估。
安全性分析基于11项临床试验中所有接受OCR的患者的综合临床和实验室数据,包括2期和3期试验的控制治疗和开放标签扩展(OLE)期,以及3b期试验VELOCE、CHORDS、CASTING、OBOE、ENSEMBLE、CONSONANCE和LIBERTO。对于选定的不良事件(AEs),使用了额外的上市后数据。严重感染(SI)和恶性肿瘤的发病率是利用多种流行病学资料进行的。
在数据截止时(2020年1月),5,680名多发性硬化症(MS)患者在临床试验中接受了OCR(18218个病人年[PY]的暴露)。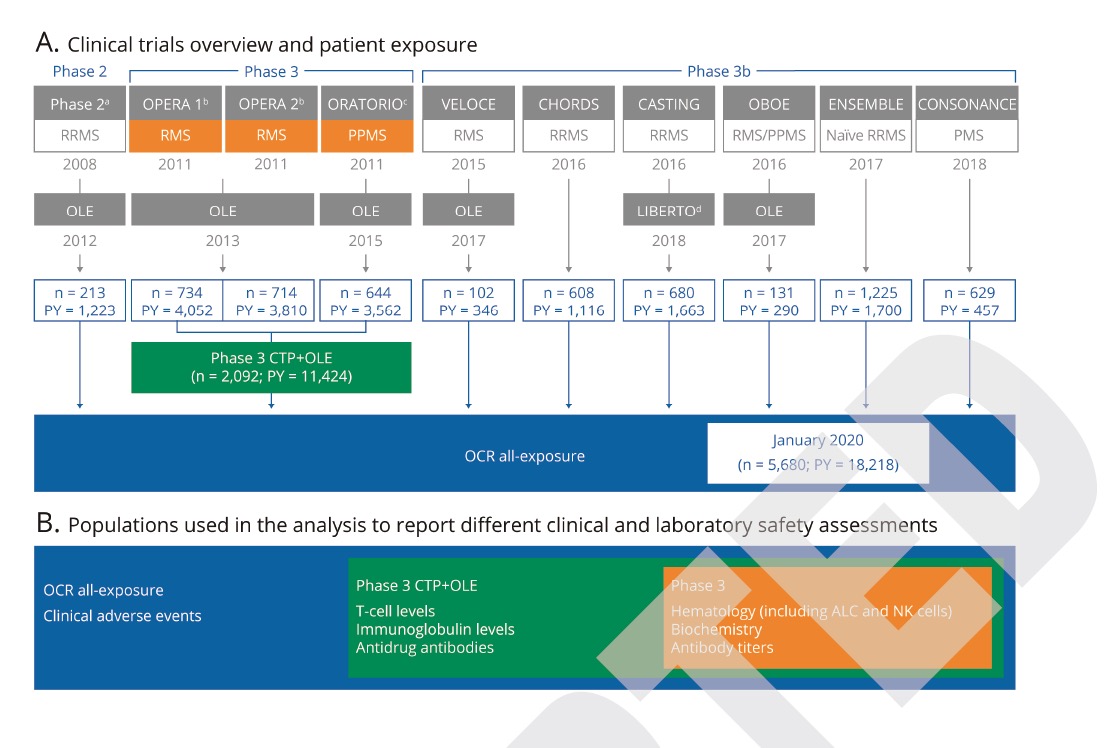
每100个PY的AEs(248;246-251)、严重AEs(7.3;7.0-7.7)、输液相关反应(25.9;25.1-26.6)和感染(76.2;74.9-77.4)的发生率(95%CI)与3期试验的控制治疗期相似。
最常见的严重AEs比率,包括SIs(2.01;1.81-2.23)和恶性肿瘤(0.46;0.37-0.57),与流行病学数据中报告的范围一致。
这个研究的重要意义在于发现 :在临床试验中连续服用OCR长达7年,以及在现实世界中更广泛地使用OCR超过3年,都与良好的和可管理的安全状况有关,在异质性MS人群中没有出现安全问题。
原文出处:
Hauser SL, Kappos L, Montalban X, et al. Safety of Ocrelizumab in Patients With Relapsing and Primary Progressive Multiple Sclerosis. Neurology. Published online September 2, 2021:10.1212/WNL.0000000000012700. doi:10.1212/WNL.0000000000012700
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#mAb#
40
#多发性#
0
#Neurol#
35
#Ocrelizumab#
0
#CRE#
42