CLIN CANCER RES:Alisertib联合利妥昔单抗或利妥昔单抗/长春新碱治疗B细胞淋巴瘤
2018-12-20 MedSci MedSci原创
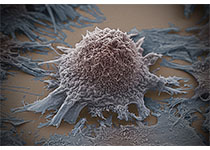
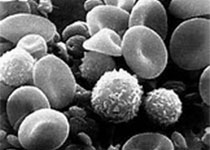
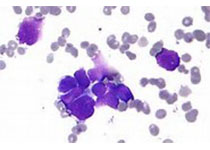
alisertib在B细胞非霍奇金淋巴瘤(B-NHL)中具有单药临床活性,与长春新碱/利妥昔单抗联合具有临床前协同作用。CLIN CANCER RES近期发表了一篇文章,研究alisertib联合使用利妥昔单抗±长春新碱治疗复发/难治性侵袭性B-NHL患者的安全性和推荐II期剂量(RP2D)。
alisertib在B细胞非霍奇金淋巴瘤(B-NHL)中具有单药临床活性,与长春新碱/利妥昔单抗联合具有临床前协同作用。CLIN CANCER RES近期发表了一篇文章,研究alisertib联合使用利妥昔单抗±长春新碱治疗复发/难治性侵袭性B-NHL患者的安全性和推荐II期剂量(RP2D)。
研究纳入患有复发/难治性,弥漫性,大B或其他侵袭性B-NHL的患者,患者在第1 天接受口服alisertib 50 mg bid 第1到7天,联合静脉利妥昔单抗375 mg / m 2,至第8天,21天循环(MR)。在随后的队列(3 + 3设计)中的患者接受增加剂量的alisertib(30mg起始剂量; 10mg增量),bid 第1到7天,联合利妥昔单抗和长春新碱[1.4mg / m 2(最大2mg)第1,8天] 8个周期(MRV)。受益的患者超过8个周期后可以继续使用单药alisertib。对保存组织进行细胞来源和MYC / BCL2 IHC检测。研究共纳入45名患者。MR的alisertib RP2D为50mg bid。MRV(n = 32)的RP2D被确定为40mg bid (40mg 时出现1例剂量限制毒性(DLT),; 50 mg 时出现2例 DLTs。89%的患者出现了药物相关的不良事件,最常见的是中性粒细胞减少症(47%)。7名患者出现完全反应(CR),7名患者出现部分反应(PR); MRV RP2D患者中有9例(45%)出现治疗反应(4例CR,5例PR),均为非生发中心B细胞(GCB)弥漫性大B细胞淋巴瘤(DLBCL)。
原始出处:
Kevin R. Kelly, Jonathan W. Friedberg, et al. Phase I Study of the Investigational Aurora A Kinase Inhibitor Alisertib plus Rituximab or Rituximab/Vincristine in Relapsed/Refractory Aggressive B-cell Lymphoma. CLIN CANCER RES. December 2018 doi: 10.1158/1078-0432.CCR-18-0286
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞淋巴瘤#
35
#利妥昔#
33
#长春新碱#
41
#Alisertib#
31
#B细胞#
28