JACC:短QT综合征小儿患者长期随访研究
2013-04-09 JACC 丁香园
短QT综合征(short QT syndrome,SQTS)是一种遗传性致死性心律失常,虽然SQTS十分少见,但其具有致死性,因此我们有必要对其进行更为深入的研究。SQTS的电生理基础是心肌细胞去极化时间缩短,导致快速性房性及室性心律失常的发生。目前研究认为SQTS与3种不同的钾离子通道及L型钙离子通道突变所致。SQTS的诊断标准是QTc间期小于340ms,SQTS目前还缺乏有效的治疗手段,ICD
短QT综合征(short QT syndrome,SQTS)是一种遗传性致死性心律失常,虽然SQTS十分少见,但其具有致死性,因此我们有必要对其进行更为深入的研究。SQTS的电生理基础是心肌细胞去极化时间缩短,导致快速性房性及室性心律失常的发生。目前研究认为SQTS与3种不同的钾离子通道及L型钙离子通道突变所致。
SQTS的诊断标准是QTc间期小于340ms,SQTS目前还缺乏有效的治疗手段,ICD可作为首选治疗,可有效预防SQTS患者发生心脏性猝死(SCD),然而由于SQTS患者年龄较小,其风险-获益比目前还不清楚。近年来,奎尼丁也用于SQTS的治疗,然而目前还缺乏用药经验。目前对于SQTS患儿的长期预后还不清楚,据此Villafane J等进行了一项临床研究,旨在探讨SQTS患儿的临床特征及长期预后。
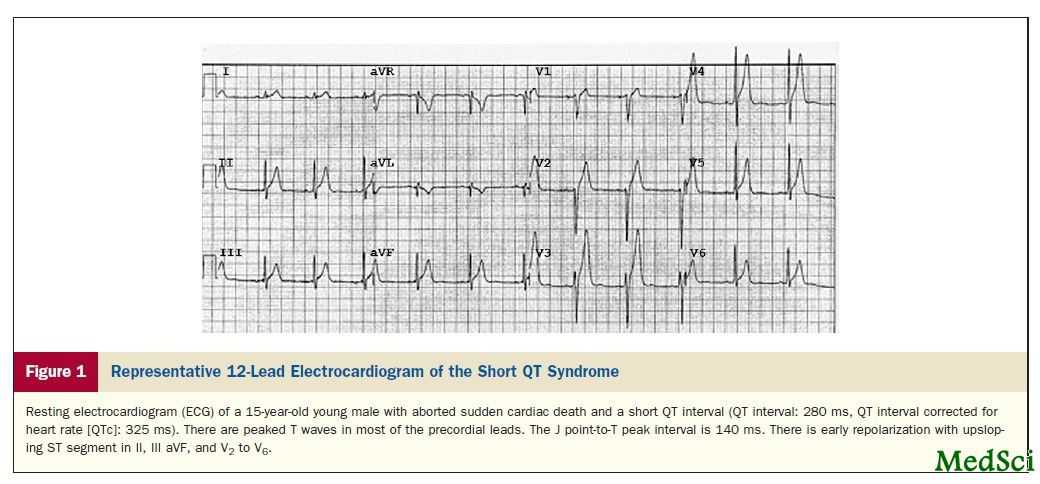
该研究的数据来自15个临床中心,分析所有患者的心电图特征、基因型、临床事件、Gollob评分及药物或ICD治疗的效果。共入选25例年龄小于21岁的患者,平均年龄为15岁,所有患者的QTc间期平均为312ms。经过平均5.9年的随访,14例患者存在临床症状,占56%,其中6例发生了心脏性猝死,占24%,4例患者出现晕厥,占16%。心律失常在SQTS患者十分常见,其中4例患者存在心房颤动,6例患者存在心室颤动,1例患者存在室上速,1例患者存在多源性室速。16例患者存在家族和个人心脏骤停病史,5例患者存在基因突变。有症状的患者Gollob评分高于无症状的患者。10例患者接受了药物治疗,主要是奎尼丁;11例患者植入了ICD,2例出现正确的放电,ICD的误放电见于64%的患者。
通过该项研究可得出以下结论:SQTS与小儿心脏性猝死相关,无症状的患者若Gollob评分<5分,提示患者无事件发生,但除外室上速的发生。Gollob评分>5分与临床事件发生相关,SQTS患者存在较高的ICD误放电率。
与心律失常相关的拓展阅读:
- Circulation:复杂性室性心律失常导管消融可改善患者长期预后
- HEART RHYTHM :致心律失常性心肌病患者或存在心肌信号传导紊乱
- 低血糖致猝死 心律失常或为始作俑者
- Clin Infect Dis :氟喹诺酮或增严重心律失常风险
- ACCF/AHA/HRS发布2012版心律失常器械治疗指南
- JBC:DES基因触发心律失常性右心室心肌病 更多信息请点击:有关心律失常更多资讯

Long-Term Follow-Up of a Pediatric Cohort With Short QT Syndrome
Objectives
The purpose of this study was to define the clinical characteristics and long-term follow-up of pediatric patients with short QT syndrome (SQTS).
Background
SQTS is associated with sudden cardiac death. The clinical characteristics and long-term prognosis in young patients have not been reported.
Methods
This was an international case series involving 15 centers. Patients were analyzed for electrocardiography characteristics, genotype, clinical events, Gollob score, and efficacy of medical or defibrillator (implantable cardioverter-defibrillator [ICD]) therapy. To assess the possible prognostic value of the Gollob score, we devised a modified Gollob score that excluded clinical events from the original score.
Results
Twenty-five patients 21 years of age or younger (84% males, median age: 15 years, interquartile range: 9 to 18 years) were followed up for 5.9 years (interquartile range: 4 to 7.1 years). Median corrected QT interval for heart rate was 312 ms (range: 194 to 355 ms). Symptoms occurred in 14 (56%) of 25 patients and included aborted sudden cardiac death in 6 patients (24%) and syncope in 4 patients (16%). Arrhythmias were common and included atrial fibrillation (n = 4), ventricular fibrillation (n = 6), supraventricular tachycardia (n = 1), and polymorphic ventricular tachycardia (n = 1). Sixteen patients (84%) had a familial or personal history of cardiac arrest. A gene mutation associated with SQTS was identified in 5 (24%) of 21 probands. Symptomatic patients had a higher median modified Gollob score (excluding points for clinical events) compared with asymptomatic patients (5 vs. 4, p = 0.044). Ten patients received medical treatment, mainly with quinidine. Eleven of 25 index cases underwent ICD implantation. Two patients had appropriate ICD shocks. Inappropriate ICD shocks were observed in 64% of patients.
Conclusions
SQTS is associated with aborted sudden cardiac death among the pediatric population. Asymptomatic patients with a Gollob score of <5 remained event free, except for an isolated episode of supraventricular tachycardia, over an average 6-year follow-up. A higher modified Gollob score of 5 or more was associated with the likelihood of clinical events. Young SQTS patients have a high rate of inappropriate ICD shocks.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JACC#
28
#随访研究#
49
#长期随访#
26
#ACC#
31
#综合征#
32