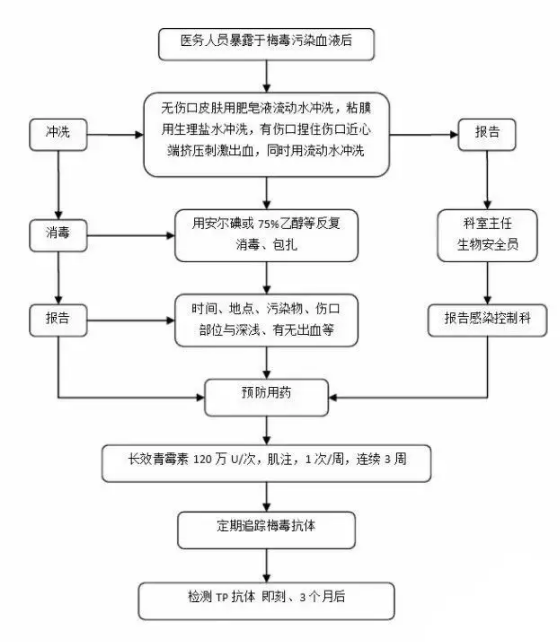
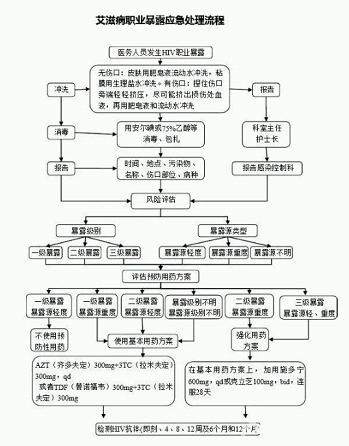
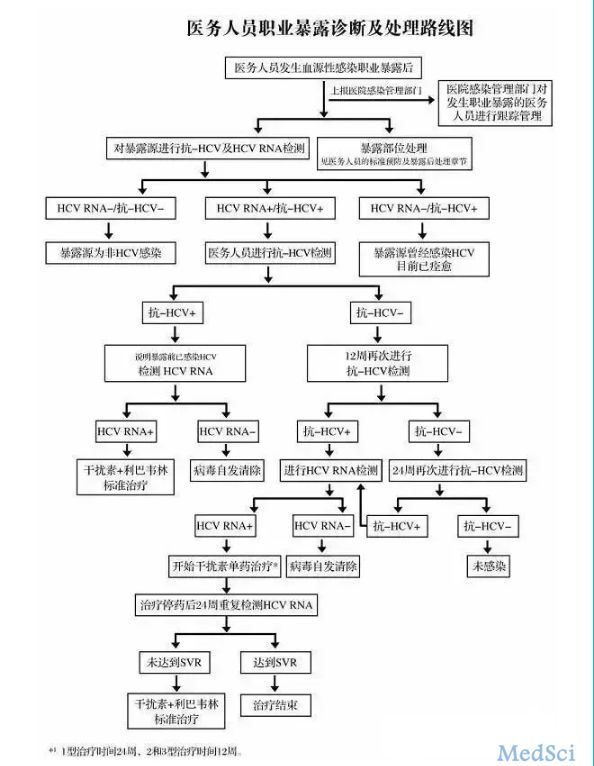
医护人员职业暴露后处理流程详解(HBV、HCV、TP、HIV)
2017-02-09 佚名 吴阶平医学基金会肝病医学部
在繁忙的医疗工作中,被针扎或接触到疑似感染者血液,是一件非常恐慌的事,接下来,我们具体讨论工作中乙肝、丙肝、梅毒、HIV职业暴露后的应付方式。医护人员职业暴露后如何处理? 1、发生职业暴露后,尽快落实紧急处理措施,并在30分钟内向护士长报告,护士长在2小时内上报预防保健科,暴露源为HIV阳性或疑似病人,应当在暴露发生后1小时内上报。 2、向上级部门报告的内容,包括损伤时

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#HBV#
34
很实用。
102
#HCV#
50
#医护人员#
50
文章不错,拜读了
101
发生职业暴露提心吊胆
74
风险风险,注意安全
82
往后要注意安全
78