JAHA:Fontan循环患者肺动脉高压疗法的效果
2021-12-21 MedSci原创 MedSci原创
PAH治疗可用于Fontan循环的成年患者。随访表明PAH治疗12个月后Fontan循环患者临床状态稳定。
先天性心脏病(CHD)手术的巨大成功之一是Fontan手术,这是一种消除单心室生理患者发绀和慢性容量超负荷的手术策略。Fontan手术在过去几十年中不断发展,改善了患者长期预后并减少了晚期并发症,尤其是在全腔静脉肺连接术(TCPC)后的患者中。然而,Fontan手术后患者的预后较差。"Fontan衰竭”是这些患者生活质量差和死亡的主要原因。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在评估英国各专科中心接受肺动脉高压(PAH)治疗的Fontan循环成年患者的数量和临床特征。
研究人员在2009年至2019年期间对英格兰和苏格兰的10个专科先天性心脏病中心确定了所有接受积极随访的Fontan循环成年患者。接受PAH治疗的患者与未接受治疗的患者相匹配。研究人员还进行了专家调查。
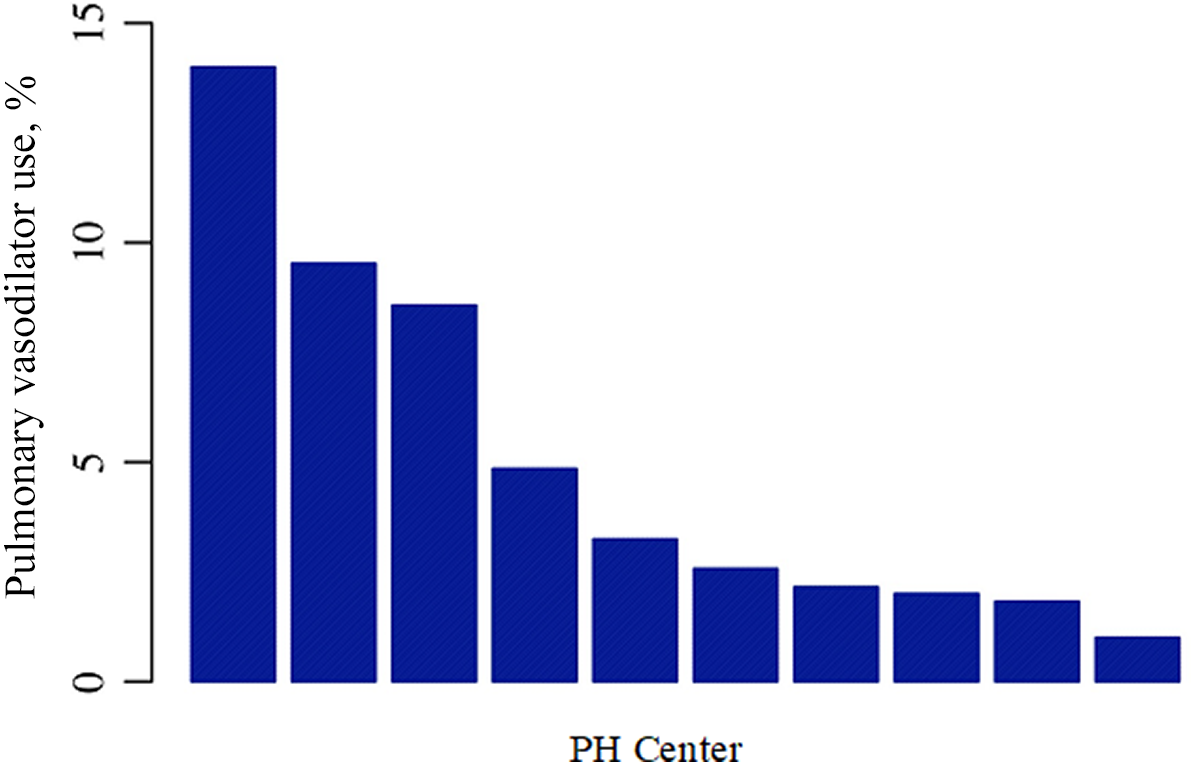
在专科中心随访的1538名Fontan患者中,只有76名(4.9%)患者在随访期间接受了PAH治疗。绝大多数(90.8%)患者接受了磷酸二酯酶5抑制剂治疗。在33%的患者中,PAH治疗是从手术后或住院期间开始的。在匹配的队列中,接受治疗的患者更有可能明显受限、有腹水、有蛋白质丢失性肠病病史或接受袢利尿剂(所有P<0.0001)。在中位随访12个月(11-15个月)后,治疗组患者的功能等级更有可能改善(P=0.01),临床参数或安全性问题没有其他变化。
由此可见,PAH治疗可用于Fontan循环的成年患者。随访表明PAH治疗12个月后Fontan循环患者临床状态稳定。
原始出处:
Andrew Constantine,et al.Use of Pulmonary Arterial Hypertension Therapies in Patients with a Fontan Circulation: Current Practice Across the United Kingdom.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.023035
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#动脉高压#
29
#Fontan#
33
#Fontan循环#
32
#AHA#
35