JCB & NCB:两篇重磅级研究揭示心血管疾病的发病机制
2016-09-30 佚名 生物谷
近日,刊登在国际杂志Nature Cell Biology和The Journal of Cell Biology的两项研究报告中,来自耶鲁大学的研究人员通过深入研究了引发心血管疾病的潜在生物学机制,相关研究或为后期新型靶向疗法的开发提供新的思路;心血管疾病是引发个体患慢性疾病及死亡的常见原因。 文章中,研究者分析了动脉粥样硬化斑块形成的过程,这种斑块能够堵塞动脉并且引发心脏病和中风的发生;
近日,刊登在国际杂志Nature Cell Biology和The Journal of Cell Biology的两项研究报告中,来自耶鲁大学的研究人员通过深入研究了引发心血管疾病的潜在生物学机制,相关研究或为后期新型靶向疗法的开发提供新的思路;心血管疾病是引发个体患慢性疾病及死亡的常见原因。
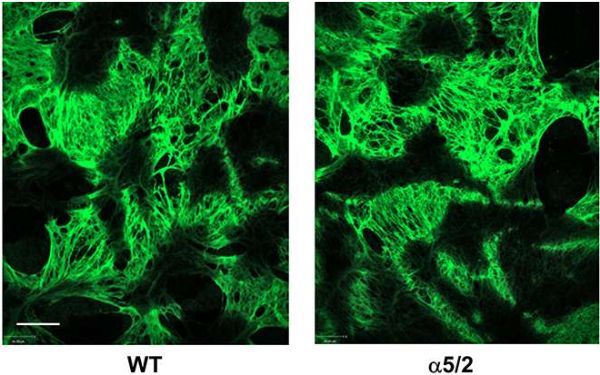
文章中,研究者分析了动脉粥样硬化斑块形成的过程,这种斑块能够堵塞动脉并且引发心脏病和中风的发生;目前对动脉粥样硬化发病机制和疗法的研究主要集中探究脂质和炎性如何诱发疾病的发生。文章中研究者Schwartz及其同事通过分析研究是否能够对动脉粥样硬化的进行重塑作用,即细胞是否能够组织中的这种结构。
研究人员研究了对细胞外基质重塑和炎症之间的关系,他们发现,在小鼠机体中,改变结合细胞外基质的受体的信号就能够减少炎症和动脉粥样硬化症的发生,同时研究者还揭示了细胞外基质的重塑如何控制机体炎症的发生,而且该研究或许能够鉴别出治疗动脉粥样硬化症的新型靶点。
在第二项研究中,研究者Anne?Eichmann对一种名为遗传性出血性毛细血管扩张症(HHT)进行了研究,这种疾病患者机体的血管处于畸形状态,从而就会引发皮肤、鼻子还有其它器官出血;HHT的发生归咎于血液中名为BMPs蛋白的两种受体发生突变所致,而在研究中研究者揭示了这些受体信号如何依赖于BMPs蛋白以及血流的力量,HHT患者血管往往并不能很好地形成,因为患者对血流量产生适当的反应。本文的研究结果或将帮助研究者们理解血管结构被调节的分子机制,同时也为寻找HHT及其它常见血管疾病的潜在治疗靶点提供了新的思路和希望。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












好文章,受益
24
#血管疾病#
24
#重磅#
27
继续关注
26
继续学习
38