君实生物完成全球抗PD-1/TGF-β双功能融合蛋白JS201临床试验首例患者给药
2021-08-02 君实生物 君实生物
该研究旨在评估JS201治疗晚期恶性肿瘤患者的安全性、耐受性、药代动力学特征及初步疗效的剂量递增、剂量扩展和临床拓展。
北京时间2021年7月30日,君实生物(1877.HK,688180.SH)宣布,公司自主研发的全球首个重组PD-1单抗/TGF-β RⅡ双功能融合蛋白(项目代号:JS201)I期临床试验(NCT04956926)已于近日完成首例患者给药。该研究旨在评估JS201治疗晚期恶性肿瘤患者的安全性、耐受性、药代动力学特征及初步疗效的剂量递增、剂量扩展和临床拓展。
由于环境和人类平均寿命延长等因素影响,癌症已成为我国人口死亡的主要原因,是公共卫生领域的一大难题。根据世界卫生组织统计[1],2020年,我国恶性肿瘤发病和死亡分别约456.9万人和300.3万人。晚期恶性肿瘤难治愈且复发率高,治疗费用居高不下,对于家庭和社会都是沉重的负担。
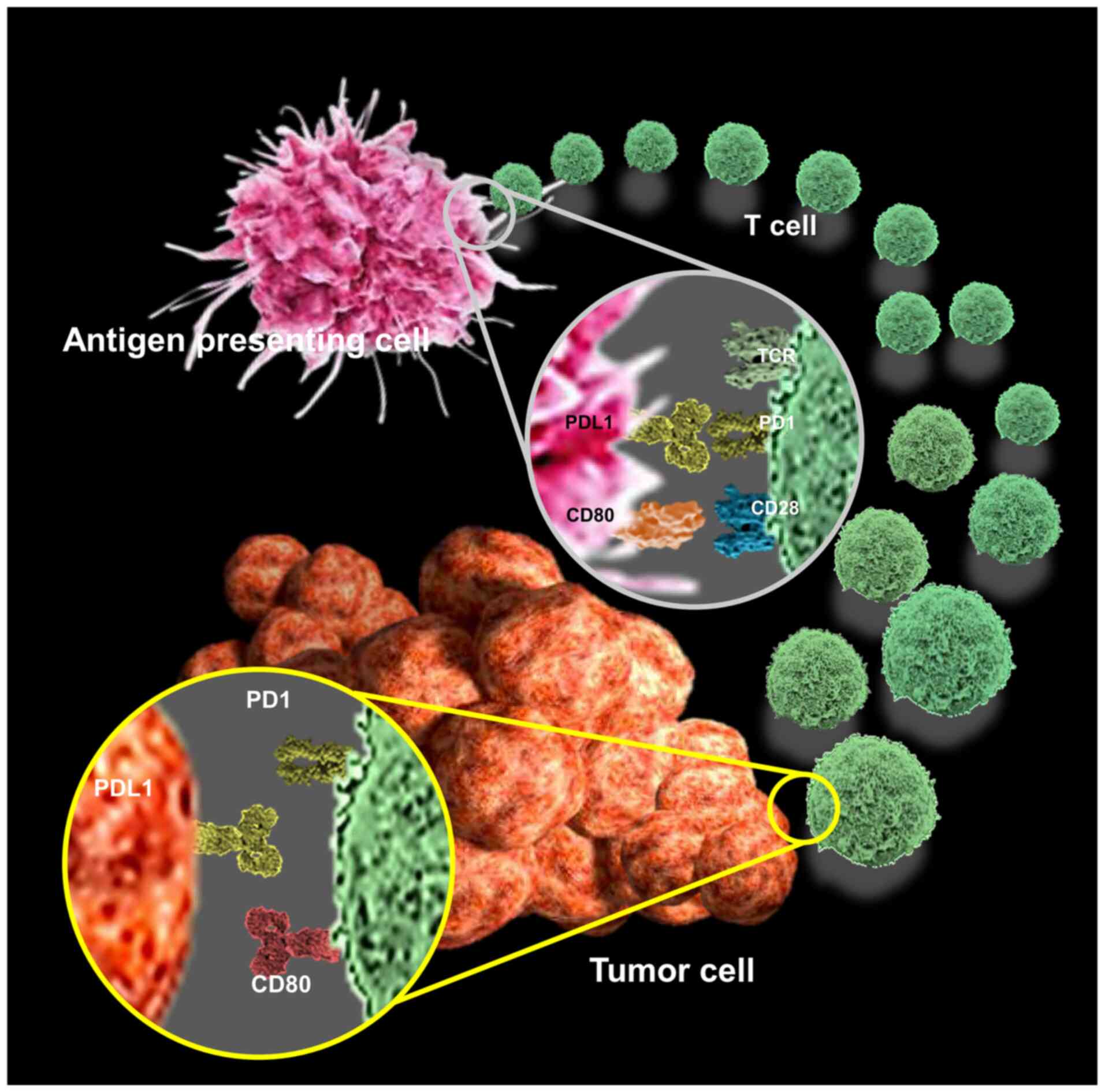
近年来,以PD-1抑制剂为代表的肿瘤免疫治疗发展迅速,已在多种恶性肿瘤中显示出显著的临床抗肿瘤活性和生存获益,不过仍有一定数量的患者无法对其产生应答。如何进一步扩大免疫疗法的受益人群并提升治疗疗效,成为该领域药物开发的重点。
相关研究发现,免疫检查点抑制剂仅作用于肿瘤及其微环境复杂系统的某一方面,而肿瘤微环境中的许多其他因素仍可介导肿瘤的免疫逃逸[2]。例如,转化生长因子-β(TGF-β)可通过促进肿瘤细胞增殖、上皮-间质转化(EMT)和新生血管生成等途径促进肿瘤的发展,并抑制肿瘤微环境中的多种免疫细胞群(包括T细胞和自然杀伤细胞)的抗肿瘤功能,进而产生“免疫排除型”的肿瘤微环境[2-4]。因此同时靶向PD-1和TGF-β,有望改善肿瘤微环境的免疫抑制状态,解除TGF-β引发的肿瘤进展,增强免疫药物的抗肿瘤活性,从而让患者获得更好的疗效。
JS201为重组PD-1单抗/TGF-β RⅡ双功能融合蛋白,靶向PD-1的单抗序列来源于君实生物自主研发的抗PD-1单抗药物特瑞普利单抗的氨基酸序列,靶向TGF-β的序列为TGF-β RⅡ胞外结构域。
临床前数据显示,JS201能够以高亲和力特异性地结合重组人PD-1及TGF-β蛋白,而且有效阻断PD-1/PD-L1或PD-1/PD-L2和TGF-β信号通路,从而激活人体免疫系统,改善肿瘤微环境,有效增强免疫应答,减少免疫逃逸及耐药性的发生。JS201作为全球首个进入临床阶段的抗PD-1/TGF-β双抗,其开发有望给肿瘤患者带来新的治疗方式,解决未被满足的临床需求。
此次开展的NCT04956926研究是一项I期、开放的、多中心临床研究,由中山大学肿瘤防治中心张力教授牵头领导,旨在评价JS201在经标准治疗进展或无标准有效治疗方案的晚期恶性肿瘤患者中的安全性、耐受性、药代动力学特征、药效学特征、免疫原性及初步有效性。研究分三个阶段:剂量递增阶段、剂量扩展阶段和临床拓展阶段。
参考文献:
1.https://gco.iarc.fr/today/data/factsheets/populations/160-china-fact-sheets.pdf
2.Lind, H., et al., Dual targeting of TGF-β and PD-L1 via a bifunctional anti-PD-L1/TGF-βRII agent: Status of preclinical and clinical advances. Journal for ImmunoTherapy of Cancer, 2020.
3.Ikushima, H., et al., TGFβ signalling: a complex web in cancer progression. Nature Reviews Cancer, 2010.
4.Tauriello DVF, et al., TGFβ drives immune evasion in genetically reconstituted colon cancer metastasis. Nature. 2018.
—— 完 ——
关于JS201
JS201是君实生物自主研发的能同时靶向PD-1和TGF-β(转化生长因子-β)的双功能融合蛋白。肿瘤微环境中PD-1和TGF-β通常会同时高表达,TGF-β通过抑制免疫反应,介导抗PD-1单抗的原发性耐药,在癌症进展中产生重要影响。因此,同时阻断PD-1和TGF-β两个免疫抑制信号可在特定的实体肿瘤中产生优化的抗肿瘤免疫反应。JS201可有效阻断PD-1/PD-L1和TGF-β免疫抑制通路,改善肿瘤微环境中的免疫调节作用,从而促进人体免疫系统对于肿瘤细胞的杀伤作用,有效增强免疫应答,减少免疫逃逸及耐药性的发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TGF#
29
#融合蛋白#
42
#TGF-β#
44
#融合#
35
肿瘤新治疗
61
且看风云
42
已读已读已读已读已读,学习学习学习学习学习,受益匪浅
47