Lancet Oncol:新辅助化疗加用尼达尼布对晚期肌肉浸润性膀胱癌患者预后的影响
2022-04-16 xiaozeng MedSci原创
在标准化疗方案中加用尼达尼布治疗肌肉浸润性膀胱癌的安全性可,但不能显著提高病理完全缓解率
指南推荐,以顺铂为基础的新辅助化疗,继以根治性膀胱切除术和盆腔淋巴结清扫术,或保留器官的放化疗作为肌肉浸润性膀胱癌的标准疗法。但是,肌肉浸润性膀胱癌新辅助化疗和根治性治疗后复发很常见。
NEOBLADE研究旨在评估在新辅助化疗中加用小分子酪氨酸激酶抑制剂尼达尼布(Nintedanib)对肌肉浸润性膀胱癌患者的缓解率和生存预后的影响。
该研究是一项平行臂、双盲、随机、安慰剂为对照的2期临床试验,招募了年满18岁、ECOG表现状态0-1分的局部晚期肌肉浸润性膀胱癌患者,随机1:1分成两组,在吉西他滨和顺铂新辅助化疗基础上加用尼达尼布(150 mg 或 200 mg,2/日,持续12周)或安慰剂。主要终点是病理完全缓解率。
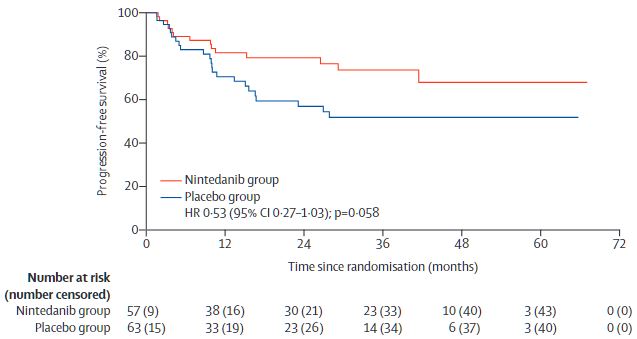
两组患者的无进展生存率
2014年12月4日至2018年9月3日,共招募了120位患者:尼达尼布组 57位、安慰剂组 63位。中位随访了33.5个月。尼达尼布组和安慰剂组的病理完全缓解率分别是37%和32%(优势比[OR] 1.25,p=0.28)。
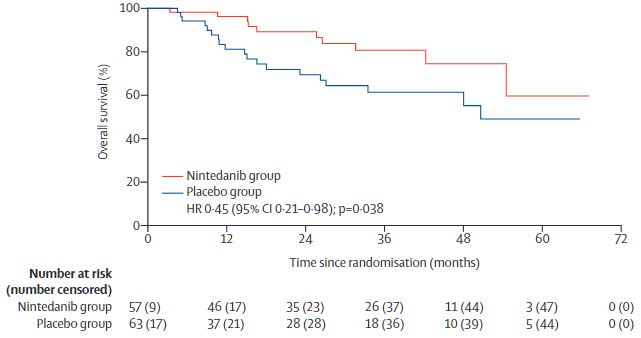
两组患者的总生存率
尼达尼布组和安慰剂组分别有53位(93%)和50位(79%)患者经历了3级及以上的毒性反应(OR 1.65, p=0.24)。最常见的3级及以上的不良反应有血栓栓塞事件(尼达尼布组 vs 安慰剂组:30% vs 21%;OR 1.63,p=0.29)和中性粒细胞计数减少(39% vs 11%;5.03, p=0.006)。此外,尼达尼布组和安慰剂组分别发生了45例和43例治疗相关的严重不良反应事件。最后,安慰剂组发生了一例治疗相关死亡(死于心肌梗死)。
总之,对于肌肉浸润性膀胱癌患者,在标准化疗方案中加用尼达尼布的安全性可,但不能明显提高病理完全缓解率。
原始出处:
Syed A Hussain, et al. Addition of nintedanib or placebo to neoadjuvant gemcitabine and cisplatin in locally advanced muscle-invasive bladder cancer (NEOBLADE): a double-blind, randomised, phase 2 trial. The Lancet Oncology. April 11, 2022. https://doi.org/10.1016/S1470-2045(22)00158-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
41
#患者预后#
55
#新辅助#
42
#Lancet#
38
坚持学习
46
lancet上果然牛,感谢梅斯更新及时
24